Functional Aspects of the Obesity Paradox in Patients with Severe Coronavirus Disease-2019: A Retrospective, Multicenter Study
Article information
Abstract
Background
Results of studies investigating the association between body mass index (BMI) and mortality in patients with coronavirus disease-2019 (COVID-19) have been conflicting.
Methods
This multicenter, retrospective observational study, conducted between January 2020 and August 2021, evaluated the impact of obesity on outcomes in patients with severe COVID-19 in a Korean national cohort. A total of 1,114 patients were enrolled from 22 tertiary referral hospitals or university-affiliated hospitals, of whom 1,099 were included in the analysis, excluding 15 with unavailable height and weight information. The effect(s) of BMI on patients with severe COVID-19 were analyzed.
Results
According to the World Health Organization BMI classification, 59 patients were underweight, 541 were normal, 389 were overweight, and 110 were obese. The overall 28-day mortality rate was 15.3%, and there was no significant difference according to BMI. Univariate Cox analysis revealed that BMI was associated with 28-day mortality (hazard ratio, 0.96; p=0.045), but not in the multivariate analysis. Additionally, patients were divided into two groups based on BMI ≥25 kg/m2 and underwent propensity score matching analysis, in which the two groups exhibited no significant difference in mortality at 28 days. The median (interquartile range) clinical frailty scale score at discharge was higher in nonobese patients (3 [3 to 5] vs. 4 [3 to 6], p<0.001). The proportion of frail patients at discharge was significantly higher in the nonobese group (28.1% vs. 46.8%, p<0.001).
Conclusion
The obesity paradox was not evident in this cohort of patients with severe COVID-19. However, functional outcomes at discharge were better in the obese group.
Introduction
The obesity paradox has been widely assessed in critical illnesses. Current evidence regarding this phenomenon suggests that obesity plays a protective role against severe critical illnesses in terms of short- or long-term survival, functional outcomes, and quality of life [1]. In coronavirus disease-2019 (COVID-19), the association between body mass index (BMI) and COVID-19 mortality remains controversial. Early in the pandemic, obesity was reported to be an essential risk factor for severity and mortality among patients with COVID-19. Moreover, several systematic reviews and meta-analyses have supported this phenomenon [2,3]. However, subsequent studies have demonstrated a positive relationship between BMI and survival in patients with severe COVID-19 [4,5]. This discrepancy implies that the obesity paradox is still not fully understood in the context of severe COVID-19.
Previously, we found that the obesity paradox in critical illnesses may be mediated by functional benefits [1]. However, the functional aspects of the obesity paradox have not been fully investigated nor characterized. Approximately 80% of patients with severe COVID-19 experience ≥1 long-term sequelae [6]. Patients who recover from severe COVID-19 experience reduced physical function, with functional impairments persisting for up to 6 months [7]. In particular, the more severe the disease, the longer the hospitalization with isolation, and the more common the impairment of physical function and exacerbation of previous functional limitations [8]. In this context, the relationship among obesity, BMI, and COVID-19 outcomes, including functional aspects, needs to be assessed. This can be an essential starting point for addressing the controversy regarding the obesity paradox in the context of severe COVID-19 and its underlying mechanisms. Accordingly, this study analyzed whether the obesity paradox is significant in patients with severe COVID-19 and respiratory failure using data from a nationwide multicenter registry and its effect on functional aspects.
Materials and Methods
1. Study population
Data regarding patients ≥19 years of age with severe COVID-19 and respiratory failure at 22 tertiary hospitals or university-affiliated hospitals from January 2020 to August 2021 were collected. This study was approved by the Institutional Review Board (IRB) of each participating hospital, including the Pusan National University Yangsan Hospital (Yangsan, South Korea) IRB (approval number: 04-2021-042; October 7, 2021). Requirements for informed consent were waived because of the minimal risk associated with a standard-of-care observational study with no interventions. COVID-19 was defined as a positive result in a real-time reverse transcription polymerase chain reaction assay to detect severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in an upper respiratory tract specimen. The following information was collected: demographic data, including age and sex; comorbidities and disease severity (sequential organ failure assessment [SOFA] score, hemodynamics, and laboratory variables at baseline); infection source and type (community- and hospital-acquired); multidrug-resistant pathogens in patients with positive cultures; treatment data; resource use; and outcome data, including 28-day and hospital mortality rates. The clinical frailty scale (CFS) was used to evaluate functional status before hospitalization and discharge. The CFS is a well-validated 9-point scale that ranges from 1 (very fit) to 9 (terminally ill), with higher scores indicating more severe frailty. The presence of frailty was divided according to CFS score: frail (CFS score 5–9) versus non-frail (CFS score 1–4).
2. Data analysis
Patients without available height or weight data were excluded from analysis (Supplementary Figure S1). Patients were divided into four groups according to initial BMI at admission: underweight (<18.5 kg/m2), normal (18.5 to 24.9 kg/m2), overweight (25 to 29.9 kg/m2), and obese (≥30 kg/m2). The primary outcome was mortality at 28 days among the four groups. The secondary outcomes were in CFS scores and frailty at discharge among the four groups. Additionally, a propensity score matching analysis was performed according to Asian BMI criteria. Patients were divided into two groups according to initial BMI at admission: obese (BMI ≥25 kg/m2) and nonobese (BMI <25 kg/m2). The propensity score was used as a balancing score to adjust for confounding variables and to determine whether obesity was associated with better patient outcomes. Therefore, the propensity score for obesity for each patient was calculated using a multivariate logistic regression model to estimate the probability of disease assignment based on the following baseline covariates: age, sex, comorbidities, CFS score, SOFA score, and treatment for respiratory failure. Obese and nonobese patients were paired at a ratio of 1:1 based on propensity scores using nearest-neighbor matching without replacement and an optimal caliper (0.1 standard deviations [SDs] of the propensity score).
3. Statistical analysis
Continuous variables are expressed as mean±SD or median and interquartile range (IQR), depending on data distribution, and were compared using the Student’s t-test or Mann-Whitney U test, as appropriate. Categorical variables are expressed as frequency and percentage and were compared using the chi-squared test or Fisher’s exact test, as appropriate. A Cox proportional hazards regression model was used to analyze clinical factors that affected death at 28 days. After univariate analysis, significant factors (p<0.05) were entered into multivariate analysis with stepwise backward selection. The risk-adjusted survival curve was plotted using the proportional hazards model and mean of the covariate method. Furthermore, a propensity score-matched (1:1) analysis was performed to compare obese and nonobese patients according to Asian BMI criteria. Propensity score matching was performed based on age, sex, comorbidities, CFS and SOFA scores, and respiratory failure treatment. SPSS version 27.0 (IBM Corporation, Armonk, NY, USA) and R version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) were used for all statistical analyses; differences with p<0.05 were considered to be statistically significant.
Results
1. Patient characteristics
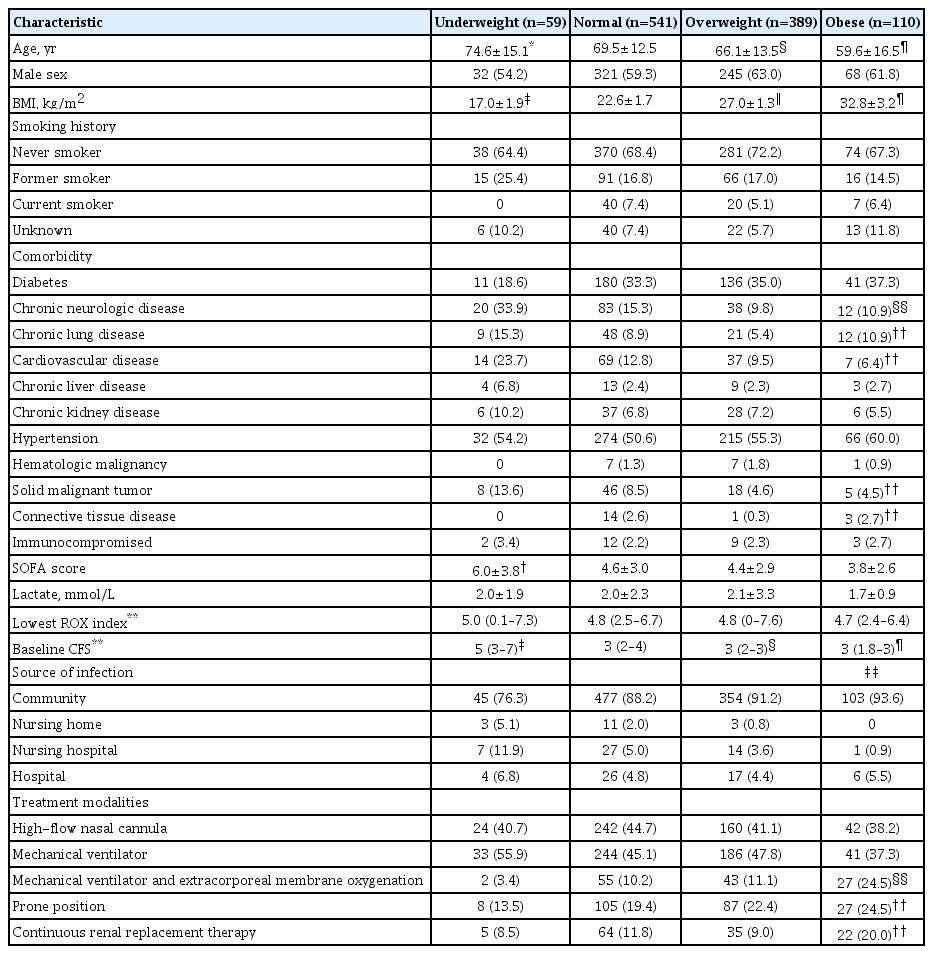
During the study period, 1,114 patients with severe COVID-19 were enrolled. Of these, 15 patients without height and weight data were excluded, and 1,099 patients were included in the final analysis (Supplementary Figure S1). A total of 468 (42.6%) patients underwent only high-flow nasal cannula, 504 (45.9%) required mechanical ventilator (MV) support, and 127 (11.6%) were treated with MV and extracorporeal membrane oxygenation (ECMO). According to the World Health Organization (WHO) BMI classification, 59 (5.4%) patients were underweight, 541 (49.2%) were normal weight, 389 (35.4%) were overweight, and 110 (10.0%) were obese. The baseline characteristics of the four groups are summarized in Table 1. Compared with the normal group, the age of the underweight group was higher (p=0.030), and the ages of the overweight group (p=0.001) and obese group (p<0.001) was lower. Compared with the normal weight group, the underweight group had a higher SOFA score (p=0.004). Compared with the normal group, the median baseline CFS score was higher in the underweight (p<0.001), but the initial CFS scores for the overweight (p=0.001) and obese (p<0.001) groups were lower. The four groups exhibited significant differences in comorbidities including chronic neurological disease(s) (p<0.001), chronic lung disease (p=0.025), cardiovascular disease (p=0.016), solid malignant tumor (p=0.017), and connective tissue disease (p=0.024). Additionally, there was a significant difference in the type of acquired infection (p=0.008). There was a significant difference in treatment with ECMO (p<0.001), continuous renal replacement therapy (CRRT) (p=0.013), and prone position (p=0.041). Data regarding initial vital signs, laboratory findings, and details of COVID-19 treatments are summarized in Supplementary Table S1.
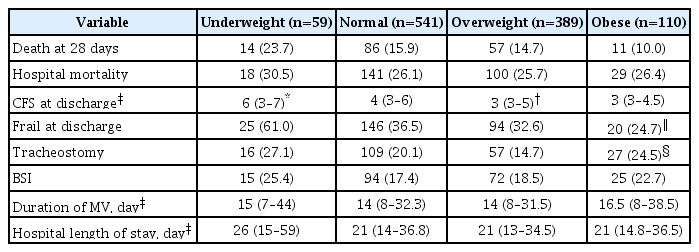
2. Clinical outcomes
There was no significant difference in mortality at 28 days among the four groups (Table 2). Compared with the normal group, the median CFS score at discharge was higher in the underweight (p=0.004) and lower in the overweight (p=0.031) groups. The obese group tended to have a lower median CFS at discharge than the normal group (p=0.064); however, the difference was not significant. There was a significant difference in the proportion of frail patients at discharge among the four groups (p=0.001). BMI was significant in the univariate Cox analysis examining death at 28 days but not in the multivariate Cox analysis (Supplementary Table S2). There was no significant difference in death at 28 days among the underweight, overweight, and obese groups compared to the normal group (Supplementary Figure S2). In the multivariate Cox analysis, age (hazard ratio [HR], 1.04; 95% confidence interval [CI], 1.02 to 1.05; p<0.001), baseline CFS score (HR, 1.30; 95% CI, 1.10 to 1.53; p=0.002), SOFA score (HR, 1.08; 95% CI, 1.03 to 1.13; p=0.001), and CRRT (HR, 2.41; 95% CI, 1.70 to 3.41; p<0.001) were significantly related to death at 28 days (Figure 1A). Kaplan-Meier curve analysis demonstrated no difference in survival according to BMI (Figure 1B).
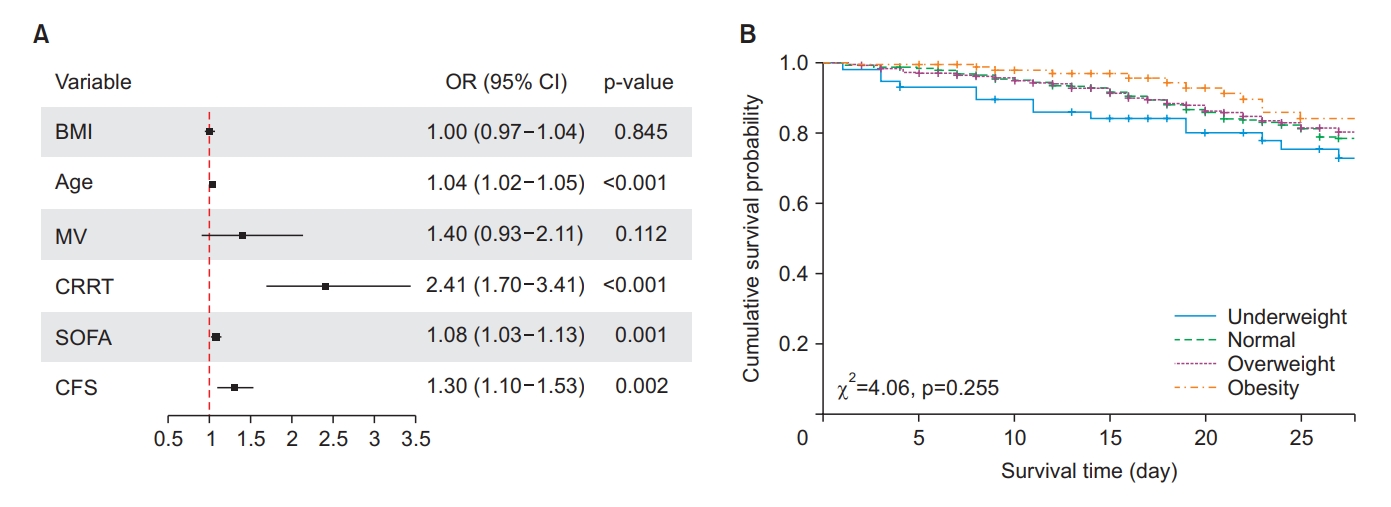
Forrest plot and Kaplan-Meier curve analysis. (A) In multivariate Cox analysis, age, baseline Clinical Frailty Scale (CFS) score, sequential organ failure assessment (SOFA) score, and continuous renal replacement therapy (CRRT) were significantly related to mortality at 28 days. (B) Kaplan-Meier curve analysis demonstrated no difference in survival according to body mass index (χ2=4.06, p=0.255). OR: odds ratio; CI: confidence interval; BMI: body mass index; MV: mechanical ventilator.
3. Propensity score matching analysis according to the Asian BMI criteria
According to the WHO Health Organization BMI classification for Asians, 499 (45.4%) patients were obese, and 600 (54.6%) were nonobese. The mean age of the obese group was lower than that of the nonobese group (65 years vs. 69.7 years, p<0.001). There was a significant difference in the type of acquired infection between the two groups (p=0.015). The median CFS score at admission was higher in the nonobese group (3 [IQR, 2 to 3] vs. 3 [IQR, 2 to 4], p<0.001). The incidence of cardiovascular disease was significantly higher in the nonobese group (8.8% vs. 13.8%, p=0.010). The proportion of chronic neurological disease(s) was significantly higher in the nonobese group (10% vs. 17.2%, p=0.001). In addition, the proportions of connective tissue disease (0.8% vs. 2.3%, p=0.046) and solid malignant tumors (4.6% vs. 9%, p=0.005) were significantly higher in the nonobese group. The mean SOFA score was significantly higher in the nonobese group (4.3 vs. 4.7, p=0.022). The proportion of those who required ECMO support was significantly lower in the nonobese group (14% vs. 9.5%, p=0.019). After propensity score matching in a 1:1 ratio, no significant differences were found between the two groups, except for BMI (Table 3). No significant differences were found in initial vital signs, laboratory findings, and detailed COVID-19 treatment between the groups after propensity score matching (Supplementary Table S3). Before propensity score matching, there was no significant difference in mortality at 28 days and hospital mortality between the two groups (Table 4). The median CFS score at discharge was higher in the nonobese group (3 [IQR, 3 to 5] vs. 4 [IQR, 3 to 6], p=0.019). The proportion of frail patients at discharge was significantly higher in the nonobese group (30.9% vs. 38.8%, p=0.019). After propensity score matching, there were no significant differences in mortality at 28 days or in-hospital mortality between the two groups. The median CFS score at discharge was higher in nonobese (3 [IQR, 3 to 5] vs. 4 [IQR, 3 to 6], p<0.001). The proportion of frail patients at discharge was significantly higher in the nonobese group (28.1% vs. 46.8%, p<0.001).
4. Risk factors for frailty at discharge in propensity-matched groups
In the univariate Cox regression analysis, age, baseline CFS score, CRRT, female sex, ECMO, BMI (≥30 kg/m2) and chronic neurological disease(s) were significantly associated with frailty at discharge (Supplementary Table S4). In the multivariate analysis, baseline CFS score (HR, 1.21; 95% CI, 1.13 to 1.31; p<0.001), female sex (HR, 1.37; 95% CI, 1.10 to 1.79; p=0.018), ECMO (HR, 1.68; 95% CI, 1.04 to 2.69; p=0.033), and BMI ≥30 kg/m2 (HR, 0.23; 95% CI, 0.09 to 0.56; p=0.001) were significantly associated with frailty at discharge.
Discussion
Results of the present study revealed that the obesity paradox in severe COVID-19 pneumonia was not evident in a cohort of East Asian patients. However, obese patients exhibited better functional outcomes on discharge after severe COVID-19. After adjusting for potential confounders using propensity score matching, the obese group exhibited significantly lower frailty at discharge than the nonobese group. The obesity paradox was evident only in the functional aspect after survival from severe COVID-19 pneumonia. The overall mortality rate was 15.3% at 28 days and 26.2% at discharge.
In the context of critical illness, the relationship between obesity and outcomes is complex and not fully understood. An ‘obesity survival paradox’ is consistent mainly for bacterial pneumonia [9,10]. However, research on the obesity paradox in viral infection has yielded mixed results. Previously, meta-analysis showed that obesity is associated with higher risks of intensive care unit admission or death in patients with influenza A (H1N1) infection [11]. Some studies have suggested that obesity may be associated with worse outcomes in severe cases of COVID-19 [12,13]. This evidence is very heterogeneous regarding population, outcome variables, and original characteristics of each virus. Conversely, there is also evidence that obesity may have a survival advantage in COVID-19 [5]. With COVID-19, we still have uncertainty in its behavior. This is the reason we were investigating this theme.
The obesity paradox has been widely approached from the perspective of metabolic benefits or protective effects against muscle wasting from critical illness. In previous studies, we showed that the obesity paradox in sepsis or refractory acute respiratory failure requiring ECMO was evident in an East Asian cohort [1]. The analysis revealed that obese patients with severe critical illness experienced better functional outcomes, including requirement(s) for MV, weaning without tracheostomy, and frailty at discharge. This implies that obesity may protect against severe loss of muscle quantity or quality from critical illness-related metabolic wasting. However, many studies investigating the obesity paradox in critical illness still report conflicting results according to the study population, underlying disease, ethnicity, and age group. The present study evaluated viral pneumonia in a cohort diagnosed with severe COVID-19 to determine whether the obesity paradox of critical illness exists within the same ethnic group.
In the present study, unlike patients with sepsis or refractory acute respiratory failure, obese patients did not exhibit better survival. Compared to the fact that obesity is a poor prognostic factor in H1N1 or seasonal influenza, there was no survival advantage in this study, and neither did the outcome deteriorate [9]. We noted a low obesity rate in this cohort, one that was lower than other Western population studies, with a BMI of 25 to 30 kg/m2 at 35.4% and a BMI >30 kg/m2 at 10% [10]. Therefore, it is unknown whether morbid obesity has adverse effects on patients with severe COVID-19, as in the United States. We performed additional propensity matching analyses to minimize the potential for confounding variables such as age, severity, and premorbidities in this cohort and to determine the effect of obesity. We found that mild obesity or overweight was not associated with increased short-term mortality after severe COVID-19 but with improved functional outcomes.
Previous studies have focused on the effects of obesity on clinical outcomes, such as hospitalization, ventilator use, and death from COVID-19; however, to our knowledge, no studies have investigated the functional outcomes of surviving patients. COVID-19 is an infectious disease that affects multiple organs and is characterized by severe inflammation and a highly catabolic state. This condition can lead to significant changes in body composition, particularly in the quantity, structure, and function of the skeletal muscles, contributing to the development of acute sarcopenia [14]. A previous study reported a 5% to 10% weight loss during the acute phase of COVID-19 for approximately 2 weeks [15]. In a study involving post-COVID-19 recoverees, the strength of the biceps brachii and quadriceps femoris was 69% and 54% of the predicted standard values in 73% and 86% of patients, respectively. The functionality of these large muscle groups was similarly impaired [16]. In this respect, overweight and mildly obese individuals have relatively better muscle retention and, may therefore, have a better functional state on discharge.
The present study had several strengths and limitations. The cohort consisted of patients of a single ethnicity with severe COVID-19. Therefore, findings of this study are not necessarily generalizable to other ethnic groups and, as such, should be interpreted with caution. Second, the COVID-19 pandemic in Korea was well controlled in terms of infectious spread, and the public health system was not overloaded, especially the critical care system, during the study period. COVID-19 data could be affected by a collapse of the healthcare system. These data were based on a robust critical care system that did not compound the outcomes of severe COVID-19. Finally, the BMI composition of the population may have limited the power of this study. Because only 2% of the cohort was morbidly obese (BMI ≥35 kg/m2), the impact of morbid obesity on severe COVID-19 is unclear. In conclusion, in severe COVID-19, unlike previous studies, an obesity paradox was not evident; however, better functional results were observed at discharge. It is difficult to rule out the possibility that the survival benefit of obesity is underpowered owing to the lack of a morbidly obese group. Nevertheless, further studies investigating this disease are required.
Notes
Authors’ Contributions
Conceptualization: Yeo HJ, Cho WH. Methodology: Kim K. Formal analysis: Kim K. Data curation: Jang JH, Park S, Lee SH, Park O, Kim TH. Validation: Yeo HJ, Cho WH. Writing - original draft preparation: Kim J, Yeo HJ. Writing - review and editing: Cho WH. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
This study was supported by the Korean Academy of Tuberculosis and Respiratory Diseases (grant number: KATRD-S-2021-2). This work was supported by a Pusan National University Research Grant (2022).
Supplementary Material
Supplementary material can be found in the journal homepage (http://www.e-trd.org).
Initial vital sign, laboratory findings, and treatment of COVID-19
Cox regression of death at 28 days
Vital signs and laboratory findings after propensity score matching
Cox regression for frailty at discharge in propensity-matched group
Flow chart of patient inclusion.
Forrest plot.