Introduction
Pneumonia is an important cause of morbidity and mortality worldwide. It is the seventh-leading cause of death in the United States, where about 915,900 episodes of pneumonia occur annually in adults aged Ōēź65 years
1. In Korea, pneumonia ranked tenth (7.1 deaths per 100,000 population) among all causes of death in 2004 and sixth (21.4 deaths per 100,000 population) in 2013
2. The incidence and direct medical costs of hospitalized pneumonia are consistently high in Korea. Persons aged Ōēź75 years, and those with underlying medical conditions, are at increased risk of hospitalization due to pneumonia
3.
Pneumonia is a frequent cause of rehospitalization after discharge; generalized vulnerability to illness also contributes to the development of acute conditions requiring rehospitalization
4.
The 30-day readmission after hospitalization for pneumonia is related to the rate of 30-day mortality after discharge
5. Moreover, pneumonia readmission rates are associated with increased medical costs and are used as an indicator of quality of care
6. Patient-, disease-, physician-, and healthcare system-related factors are associated with pneumonia readmissions and are targets of interventions to reduce the rate of readmission for pneumonia
7. Clinically, identification of the reasons and risk factors for readmission is important for discharge planning.
The rates, reasons, and risk factors for pneumonia readmission vary among populations, regions, and methodologies. Most prior readmission studies were conducted in North America and Europe. One Korean study assessed only healthcare system-related factors in elderly (age Ōēź65 years) pneumonia patients using nationwide data
6. Although pneumonia is a frequent cause of readmission, which is related to several modifiable factors, few Asian studies have investigated hospital readmission for pneumonia. Here we evaluated the rates, reasons, and risk factors for 30-day readmission following hospitalization for community-acquired pneumonia (CAP) in the general adult population of Korea.
Discussion
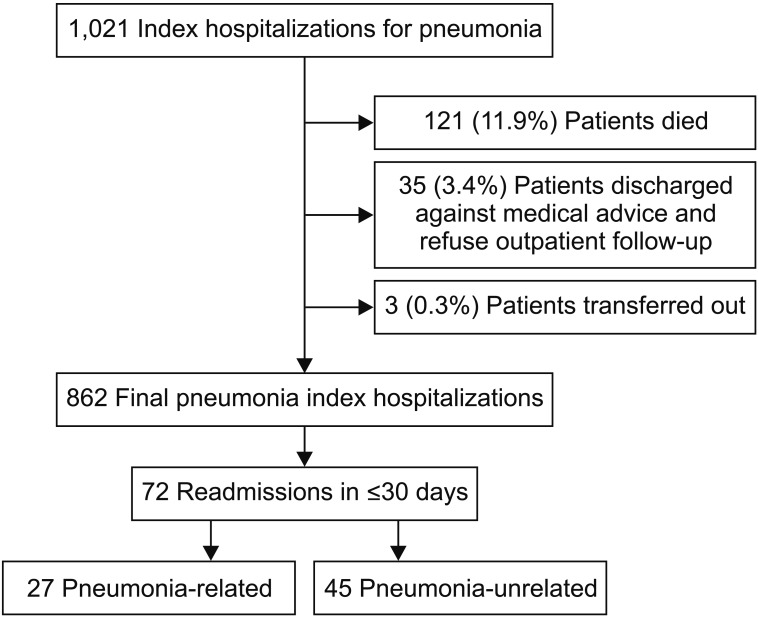
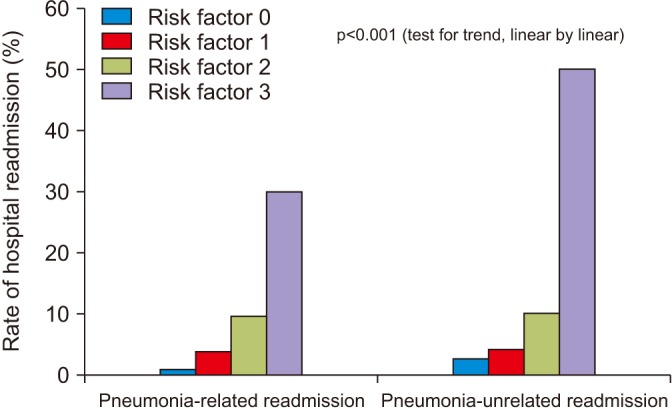
In this study, of the 862 patients hospitalized for CAP, 72 (8.4%) were readmitted within 30 days following hospital discharge. Pneumonia-related and -unrelated causes accounted for 37.5% and 62.5% of the total readmissions, respectively. The risk factors for pneumonia-related readmission (para/hemiplegia, malignancy, PSI class Ōēź4, and clinical instability Ōēź1 at hospital discharge) were different from those for pneumonia-unrelated readmission (chronic lung disease, chronic kidney disease, treatment failure, and decompensation of comorbidities). Moreover, the likelihood of hospital readmission increased with increasing number of risk factors.
Several studies performed in the United States and Europe have assessed readmission for pneumonia
13,15,16,17. In South Korea, the number of physicians per bed is reportedly associated with readmission of elderly CAP patients
6. However, this study included only patients >65 years and did not assess demographic or disease-specific factors. To our knowledge, ours is the first Asian study to evaluate risk factors for hospital readmission following discharge of general adult patients (age Ōēź18 years) hospitalized for CAP.
The all-cause 30-day readmission rate after hospitalization for pneumonia was 8.4%, compared to 7.3%-18.3% in prior works
4,13,18. In a systematic chart review, the pooled all-cause 30-day readmission rate was 11.6%. Generally, US-based studies and those involving elderly patients (age Ōēź65 years) show higher rates of all-cause 30-day readmission than non-US-based studies and those involving adults (age Ōēź18 years)
19. The all-cause 30-day readmission rate in our study was similar to the values reported by non-US-based studies and those not restricted to elderly patients
13,18. A prior work involving elderly patients (age >65 years) in South Korea reported a higher (19.1%) all-cause 30-day readmission rate than our finding
6. Thus, the healthcare environment (including hospital accessibility, financial issues, and medical practices) and age are important determinants of readmission rates.
The leading causes of 30-day readmission in our study were pneumonia (37.5%), pulmonary disease (20.8%), gastrointestinal disease (18.1%), and cardiovascular disease (5.6%). Pneumonia, heart failure/cardiovascular disease, and chronic obstructive pulmonary disease/pulmonary disease are the leading reasons for hospital readmission within 30 days
19. Interestingly, gastrointestinal causes were the third-mostfrequent reasons for hospital readmission. This is higher than in previous reports, possibly because of the effect of the large proportion (63.7%) of high-risk (PSI class Ōēź4) patients on the incidence of gastrointestinal bleeding and
Clostridium difficile-associated diarrhea (CDAD) (8 cases/all 13 gastrointestinal causes)
13,15,18. Indeed, seven of the eight patients (87.5%) who developed gastrointestinal bleeding and CDAD were in the high-risk group (PSI class Ōēź4).
Para/hemiplegia and malignancy were associated with pneumonia-related readmission. This may be because patients with these comorbidities have decreased performance status and/or immunity. Among patients readmitted for pneumonia-related reasons, 44.4% (12/27) had aspiration pneumonia associated with comorbidities. Indeed, the aspiration risk is reportedly associated with higher rates of readmission and recurrent pneumonia in patients with CAP
20. Thus, evidence-based interventions, such as angiotensin-converting enzyme inhibitors
21,22, could prevent readmission for recurrent aspiration pneumonia in high-risk patients. Moreover, maintaining good oral hygiene, withholding unnecessary medications, food thickening, sitting upright while eating, head elevation of at least 30┬░, and swallowing rehabilitation might decrease the risk of aspiration in high-risk patients
23. Education of patients regarding these interventions before hospital discharge would decrease the pneumonia-related readmission rate.
PSI class ŌēźIV and clinical instability at hospital discharge were risk factors for pneumonia-related readmission. Unlike previous studies
15,16,18, our findings revealed that PSI class ŌēźIV is an independent risk factor for pneumonia-related readmission. However, those prior works did not separate pneumoniarelated and -unrelated readmissions. We found that a clinical instability score of Ōēź1 was an independent risk factor for readmission, in accordance with previous reports
13,17. Discharge at the optimal time (taking into consideration clinical stability) could prevent pneumonia-related readmission, especially in high-risk patients (PSI class ŌēźIV). Despite clinical instability, there may be concerns about being discharged from the hospital in this study. However, it is thought that there might have been cases of stable conditions that could be discharged clinically but belonging to clinical instabilities defined in our study. In addition, many patients transferred to secondary hospitals due to comorbidities, so it is thought that there have been cases of step down referral with some clinical instability. Neither the presence of a multidrug-resistant (MDR) pathogen nor IIAT was associated with pneumonia-related readmission.
We found that comorbidities such as chronic lung disease and chronic kidney disease, treatment failure, and decompensation of comorbidities (as in a prior report
13) were associated with pneumonia-unrelated readmission. This is because pneumonia promotes inflammation and dysregulates the immune response, leading to progression of comorbidities. Also, decompensation of comorbidities during hospitalization doesn't recover well even after being discharged from the hospital, leading to the possibility of rehospitalization. In particular, the proportion of patient with chronic lung disease in our study is high, the acute exacerbation of chronic lung disease caused by pneumonia is thought to have influenced on rehospitalization. Disease severity, presence of an MDR pathogen, and IIAT were not associated with pneumonia-unrelated readmission.
This study had several limitations. First, because it was a retrospective study conducted at a single center, the results cannot be generalized. Second, we did not assess readmissions to other hospitals; we attempted to overcome this limitation by excluding patients who refused outpatient follow-up. However, the number of patients who required readmission could have been underestimated. We believe that a multicenter, prospective study is required in order to assess the causes of readmission in patients with pneumonia. Third, we focused on patient-related factors as determinants of readmission. Physicians' admission decisions and healthcare-system factors are associated with hospital readmissions but were not investigated because of a lack of information. Fourth, the investigation of patients who died within 30 days after discharge was difficult, and there was lack of analysis.
In conclusion, we found that 8.4% of the patients hospitalized for CAP were rehospitalized within 30 days of discharge. This is generally consistent with previous studies involving different populations, regions, and methodologies. Pneumoniarelated and -unrelated causes accounted for 37.5% and 62.5%, respectively, of the total readmissions. The risk factors for pneumonia-related and -unrelated readmission were different. Strategies to prevent aspiration and to achieve clinical stability at hospital discharge, especially in patients with PSI class ŌēźIV, para/hemiplegia, or malignancy could prevent pneumonia-related readmission to hospital. Appropriate management of comorbidities in high-risk patients (i.e., those with chronic lung disease and chronic kidney disease) would reduce the pneumonia-unrelated readmission rate. Therefore, aspiration prevention, discharge at the optimal time, and close monitoring of comorbidities may reduce the frequency of readmission among patients with CAP.






 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



