pncA Mutations in the Specimens from Extrapulmonary Tuberculosis
Article information
Abstract
Background
Pyrazinamide (PZA) is an effective antitubercular drug that becomes toxic to Mycobacterium tuberculosis when converted to pyrazinoic acid by pyrazinamidase (PZase), encoded by mycobacterial pncA. A strong association was noted between the loss of PZase activity and PZA resistance. The causative organisms in extrapulmonary tuberculosis are rarely cultured and isolated. To detect pncA mutations in specimens from extrapulmonary tuberculosis as confirmative diagnosis of mycobacterial infection and alternative susceptibility test to PZA.
Methods
Specimens were collected from clinically proven extrapulmonary tuberculosis. pncA was sequenced and compared with wild-type pncA.
Results
pncA from 30 specimens from 23 donors were successfully amplified (56.6% in specimens, 59% in donors). Six mutations in pncA were detected (20.0% in amplified specimens, 26.1% in specimen donors) at nucleotide positions of 169, 248 and 419. The mutation at position 169 results in substitution of aspartic acid for histidine, a possible allelic variation of M. bovis that have intrinsic PZA resistance. The mutation at position 248 changes proline into arginine and that at position 419, arginine into histidine.
Conclusion
DNA-based diagnosis using pncA may be simultaneously useful for the early diagnosis of mycobacterial infection and the rapid susceptibility to PZA in extrapulmonary tuberculosis. A potential implication of pncA allelic variation at 169 might be suggested as a rapid diagnostic test for M. bovis infection or Bacille Calmette-Guérin (BCG) reactivation.
Introduction
Pyrazinamide (PZA) is one of the effective antitubercular drugs. When combined with the first-line drugs isoniazid and rifampicin, it shortens the duration of antitubercular treatment1. PZA becomes toxic to Mycobacterium tuberculosis when converted to pyrazinoic acid by pyrazinamidase (PZase), which is encoded by mycobacterial pncA. Loss of enzymatic activity by mutation is considered to be the main mechanism responsible for PZA resistance, and extensive investigation of the patterns of pncA mutation have demonstrated a strong correlation between loss of PZase activity and PZA resistance in M. tuberculosis2-11.
The drug susceptibility test to PZA is complicated and time consuming, especially when the mycobacterial isolates are hardly cultured1,12. In pulmonary tuberculosis, because of the high concentration of tubercle bacilli in sputa and bronchoalveolar lavage specimens, it is relatively easy and convenient to collect appropriate isolates for mycobacterial culture. However, in extrapulmonary tuberculosis, the isolates are rarely cultured when the specimens are collected from an infected tissue biopsy or body fluid that contains small numbers of bacilli13-17. The diagnosis of extrapulmonary tuberculosis can be made from histologic findings or recently by molecular-based methods using polymerase chain reaction (PCR), where some drug susceptibility testing can also be performed4,13,17-19.
We postulated that the detection of mycobacterial pncA in the specimens might not only rapidly confirm the diagnosis of M. tuberculosis infection, but also simultaneously determine the drug susceptibility to PZA by sequencing, substituting the traditional susceptibility tests depending on mycobacterial culture. We investigated pncA mutations in specimens from the cases of clinically proven extrapulmonary tuberculosis.
Materials and Methods
1. Specimens from extrapulmonary M. tuberculosis infection
The extrapulmonary mycobacterial samples were collected from Seoul National University Hospital, Seoul, Korea from 2001 to 2005 and Jeju National University Hospital, Jeju, Korea from 2005 to 2007, with information on the origin of the specimens and the presumptive diagnosis. Specimens were separated into aliquots and stored at -80℃. Some specimens that were later clinically proven to be other than mycobacterial infection were excluded.
2. PCR of pncA
DNA from each specimen was extracted by a previously described method20, and pncA including the promoter region was amplified by PCR using the GeneAmp PCR system 9600 (PerkinElmer, Foster City, CA, USA), with the primers 5'-GGCGTCATGGACCCTATATC-3' and 5'-CAACAGTTCATCCCGGTTC-3'. The PCR parameters were 5 minutes at 95℃, followed by 40 cycles of 45 seconds at 94℃, 45 seconds at 60℃ and 60 seconds at 72℃, with termination using a final extension step at 72℃ for 10 minutes. The PCR product of 690 bp was purified using QIAEX II Gel Extraction Kit (QIAGEN Inc., Mainz, Germany) according to the manufacturer's instructions, and sequenced by BigDye Terminator cycle sequencing kit with AmpliTaq DNA polymerase (Applied Biosystems, Foster City, CA, USA). The PCR techniques were validated in the previous study11.
3. Sequencing for comparison with wild-type pncA
Nucleotide sequences were analyzed using BioEdit software version 5.0.9.1 (Ibis Biosciences, Carlsbad, CA, USA), Chromas version 2.33 (http://www.technelysium.com.au), and Basic Local Alignment Search Tool (http://blast.ncbi.nlm.nih.gov). Mutations in pncA coding regions were defined as any allelic difference leading to translational changes in PZase or changes in the promoter region compared with those in the PZA-susceptible strain of M. tuberculosis, H37Rv (ATCC 25618).
Results
Fifty three specimens were collected from infected tissues and body fluids, from 39 patients diagnosed with extrapulmonary tuberculosis such as osteomyelitis, spondylitis, arthritis, lymphadenitis, meningitis, and pericarditis. In 30 specimens (56.6%) from 23 patients (59.0%), the pncA coding region including the promoter was successfully amplified by PCR. The sequenced DNA from each specimen was compared with that of wild-type M. tuberculosis H37Rv. Three identical mutations in pncA were detected in 6 specimens from 6 patients (20.0% of amplified specimens, 26.1% of specimen donors), while the sequences in 24 specimens from 17 patients were identical to that of the wild type (Table 1).
All the mutations showed single point mutations where a single nucleotide was changed, subsequently translating into a different amino acid in PZase protein. The mutations were detected at nucleotide positions of 169, 248, and 419 from the start codon (ATG) of pncA. The mutation at position 169 detected in four specimens was identical, a change of C to G, which caused a change from histidine (CAC) to aspartic acid (GAC) at amino acid position 57 of PZase. The mutation at nucleotide position 248 detected in one specimen changes amino acid 83 from proline (CCC) to arginine (CGC). One specimen showed a mutation at nucleotide 419, which changes arginine 140 (CGC) into histidine (CAC) (Figure 1).
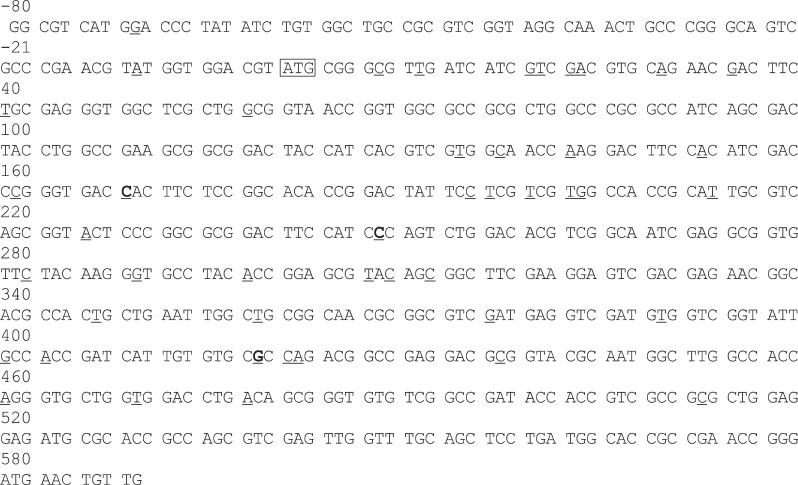
Genomic DNA sequences of pncA encoding pyrazinamidase in Mycobacterium tuberculosis. The mutation spots in pncA in pyrazinamide (PZA)-resistant isolates previously reported in the reference 6-8,11 among South Koreans were underlined. Three mutations from extrapulmonary tuberculosis detected in this study were marked in bold. Nucleotides were numbered from start codon  of pncA. This figure is modified from those of the reference7,11.
of pncA. This figure is modified from those of the reference7,11.
Discussion
In extrapulmonary tuberculosis, the mycobacteria are rarely cultured because of the limited numbers of living germs in the clinical specimens. In this study, PCR amplification of mycobacterial pncA was successful in around 60% of the specimens, that is, identification of mycobacterium in the specimens, where the sensitivity of the PCR techniques were validated in over 99% in the previous study11. PCR-based diagnosis of mycobacterial infection in extrapulmonary tuberculosis might be far more sensitive than the traditional mycobacterial culture, in case the results of the culture are compared. The limitation of this study is that the detailed clinical information was neither available nor accessible retrospectively. The information from each subject on the host immune status, the result of mycobacterial culture and susceptibility test to PZA, and the response to the treatment should have been compared with the results of the PCR-based identification of pncA mutations.
In the treatment of M. tuberculosis infection, recognition of drug susceptibility is important and even urgent, especially where the bacteria are resistant to one or both of isoniazid and rifampicin. The standard method to test susceptibility of M. tuberculosis to PZA takes at least 4~8 weeks of mycobacterial culture in Löwenstein-Jensen medium, after which the PZase activity is measured using Wayne's method12. In the standard treatment for tuberculosis, PZA is used usually in the first two months to reduce the duration of treatment required1. Although in South Korea around 10% of the mycobacterial isolates are resistant to PZA, the results of the traditional drug susceptibility test to PZA provide little information that can inform treatment decisions21. However, thanks to the molecular diagnosis using PCR, the susceptibility results with high sensitivity can be promptly obtained without the necessity for culture of the isolates17,22. Because of the low culture rates for samples obtained from extrapulmonary tuberculosis, molecular drug susceptibility tests are advantageous. Yun et al.20 reported that in osteoarticular tuberculosis, susceptibility tests using PCR amplification and sequencing of rpoB to detect mycobacterial drug resistance to rifampicin were efficient. Because of the limited numbers of bacteria in joint biopsy specimens, the isolates were hardly cultured.
Although more understanding is required of the mechanism of defective PZase activity in strains with wild-type pncA, drug resistance to PZA was reported in 80% to 90% of isolates with pncA mutations5,10,23. Detection of mutations in the pncA coding region is a promising and rapid drug susceptibility test, especially when isolates are not cultured.
In this study, three different mutations in six specimens were identified at nucleotide position of 169, 248, and 419 in pncA. C to G substitution at nucleotide 169 in pncA reported in three M. bovis strains and three Bacille Calmette-Guérin (BCG) substrains2,24. It had been identified in the previous studies of Korean subjects7, which should have been confirmed as either a substitution mutation resulting in defective PZase activity in M. tuberculosis, or an allelic variation of M. bovis including BCG that have intrinsic PZA resistance2,24,25. The results were not described in this study, because of the failure in PCR amplification with other primers described either for M. tuberculosis or M. bovis25. The limitation of this study is lacking of the donors' clinical information regarding systemic status of host immunity. Out of four cases of mutation at 169, two were marked under 2 years old, one human immunodeficiency virus positive, and one aged at 72. Some disseminated M. bovis infection has been reported in immunocompromized infants and in patients with late-stage acquired immune deficiency syndrome26-30. There is a strong possibility that some of the 4 patients diagnosed with extrapulmonary tuberculosis might have reactivation of the BCG vaccination. The adverse reactions of the same BCG strain were systemically reviewed in Taiwan, but not in Korea31.
The mutation at nucleotide 419 (amino acid R140H) of pncA was described in five different strains of 36 multidrug-resistant M. tuberculosis isolates in Japan10. These, however, showed intact PZase activity and no PZA resistance, which suggests that the mutation has no influence on the enzyme activity. We failed to find any previous reports of a mutation at nucleotide 248 (C to G substitution). This might be a newly discovered mutation, but because of the limited numbers of cases in our study, we cannot determine the importance of the mutation or its propagation in emerging drug resistance in M. tuberculosis11.
In conclusions, DNA-based diagnosis using pncA may be simultaneously useful for the early diagnosis of mycobacterial infection and the susceptibility to PZA, especially in specimens from extrapulmonary tuberculosis where the isolates are rarely cultured. A potential implication of pncA allelic variation at 169 is suggested as a rapid diagnostic test for M. bovis infection or BCG reactivation, which was not confirmed in this study because of limited clinical information.
Acknowledgements
This work was supported partly by a research grant from Jeju National University Hospital in 2011.
