First Outcome of MDR-TB among Co-Infected HIV/TB Patients from South-West Iran
Article information
Abstract
Background
Tuberculosis (TB) is the leading cause of mortality among human immunodeficiency virus (HIV) patients and the majority of them occur in developing countries. The aims of the present study were to determine the frequency of HIV/TB co-infection and other probable associated factors.
Methods
This 10 year retrospective study was conducted on 824 HIV patients in the south-west of Iran. HIV infection was diagnosed by the enzyme linked immunosorbent assay and confirmed by Western blot. TB diagnosis was based on consistency of the clinical manifestations, chest X-ray, and microscopic examination. Drug susceptibility testing was done by the proportional method on Löwenstein-Jensen media.
Results
Of 824 HIV patients, 59 (7.2%) were identified as TB co-infected and the majority (86.4%) of them were male. Of the overall TB infected patients, 6 cases (10.2%) showed multidrug-resistant with the mean CD4+ lymphocyte count of 163±166 cells/mm3. The main clinical forms of TB were pulmonary (73%). There was a significant (p<0.05) correlation between TB infection and CD4+ lymphocyte counts ≤200 cells/mm3, gender, prison history, addiction history, and highly active anti-retroviral therapy.
Conclusion
We reported novel information on frequency of HIV/TB co-infection and multidrug resistant-TB outcome among co-infected patients that could facilitate better management of such infections on a global scale.
Introduction
Tuberculosis (TB), as one of the oldest human health threatening diseases, is still considered as one of the most important causes of morbidity and mortality on a global scale1. However, the situation becomes far worse when TB co-infection with human immunodeficiency virus (HIV) occurs. TB is the leading cause of mortality in HIV seropositvie patients, accounting for about 26% of acquired immune deficiency syndrome (AIDS)-related deaths and the majority of them occur in developing countries23. In 2012, the World Health Organization (WHO) estimated over one million people worldwide with TB/HIV co-infection4.
While more than two million new cases of HIV infection occur per year3, recent estimates suggested that more than 90,000 HIV positive people are living in Iran5. The reports by WHO indicate that the occurrence of new active cases of TB per year is approximately 9 million around the world6. Based on WHO reports, the incidence rate of TB for Iranians in 2012 was 21 cases per 100,000 inhabitants. Neighboring with high TB burden countries is one of the fundamental challenges for our country7. One of the greatest threats in management of TB is that about 50 million persons are infected with multidrug-resistant TB (MDR-TB) and most of them are reported from developing countries8. Iran is one of these countries that has not previously even reported MDR-TB, also shown prevalence of extensively drug-resistant TB910.
It has been reported that up to 10% of HIV/TB co-infected patients develop active TB11. Active TB can occur at any stage of HIV disease, although it mainly depends on the immunosuppression level11. Although cell mediated immunity is necessary for TB infection control, CD4+ T lymphocytes role seems to be more critical3. Depletion of CD4+ T cells, which is a main consequence of AIDS, has an important risk in progress of active TB3. Aprroximatly, 10% of people who are only infected with TB will develop active TB disease3. However, in HIV positive patients compared to people without HIV, there is a significant increased in relative risk of developing active TB6. Depletion of CD4+ T cells increases the chance of TB dissemination and frequency of extra-pulmonary TB in HIV patients12. The CD4+ T cells have an essential role in generation of granulomas and subsequently limiting the TB infection6.
Since immune compromised patients are more vulnerable to acquiring TB infection or reactivation, diagnosis of TB in HIV positive patients is the priority to prevent increased spread of TB3. The aims of the present study were to determinate the frequency of TB co-infection among HIV patients and other probable factors affecting this situation in the south-west of Iran.
Materials and Methods
1. Study setting and design
This 10-year retrospective study was conducted on all active HIV patients who referred to Shiraz HIV/AIDS Research Center from 2004 to 2013. Shiraz HIV/AIDS Research Center as the second HIV/AIDS Research Center in Iran is affiliated to Shiraz University of Medical Sciences, located in Shiraz, the south-west of Iran. Shiraz HIV/AIDS Research Center is run by research, education and counseling HIV/AIDS experts.
This study was approved by the Ethics Committee of Shiraz University of Medical Sciences. The ethics committee waived the need for informed consent because we were to use medical records. It did not harm any of the patients and the patients' personal details were kept strictly secure and confidential.
2. Study population
The population of this study consisted of 824 HIV positive patients with an active profile in database of Shiraz HIV/AIDS Research Center. In this study, we had no restrictions for including patients; the only exclusion criterion was a lack of medical records.
3. Diagnosis of HIV and TB infections
Primary HIV infection was diagnosed by the enzyme linked immunosorbent assay (ELISA). Firstly, positive ELISA results were then confirmed by a Western blot test. TB was routinely diagnosed by the consistency of the clinical manifestations, chest X-ray, and microscopic examination of the sputum smear and/or culture. The cases suspicious of extra-pulmonary TB underwent tissue biopsy. The final diagnosis was based on histological findings such as caseating granuloma or acid fast bacilli (AFB) in tissue samples. Drug susceptibility testing was done by the proportional method on Löwenstein-Jensen media and resistance to isoniazid and rifampin, considered as MDR-TB.
Demographic data, such as age, gender, prison history, addiction history and transmission route, were obtained from all patients. Clinical information such as CD4+ lymphocyte count was also evaluated.
Statistical analysis was performed using SPSS software version 19.0 (IBM Corp., Armonk, NY, USA). Chi-square and t tests were conducted to analyze the results. p<0.05 was considered as statistical significance.
Results
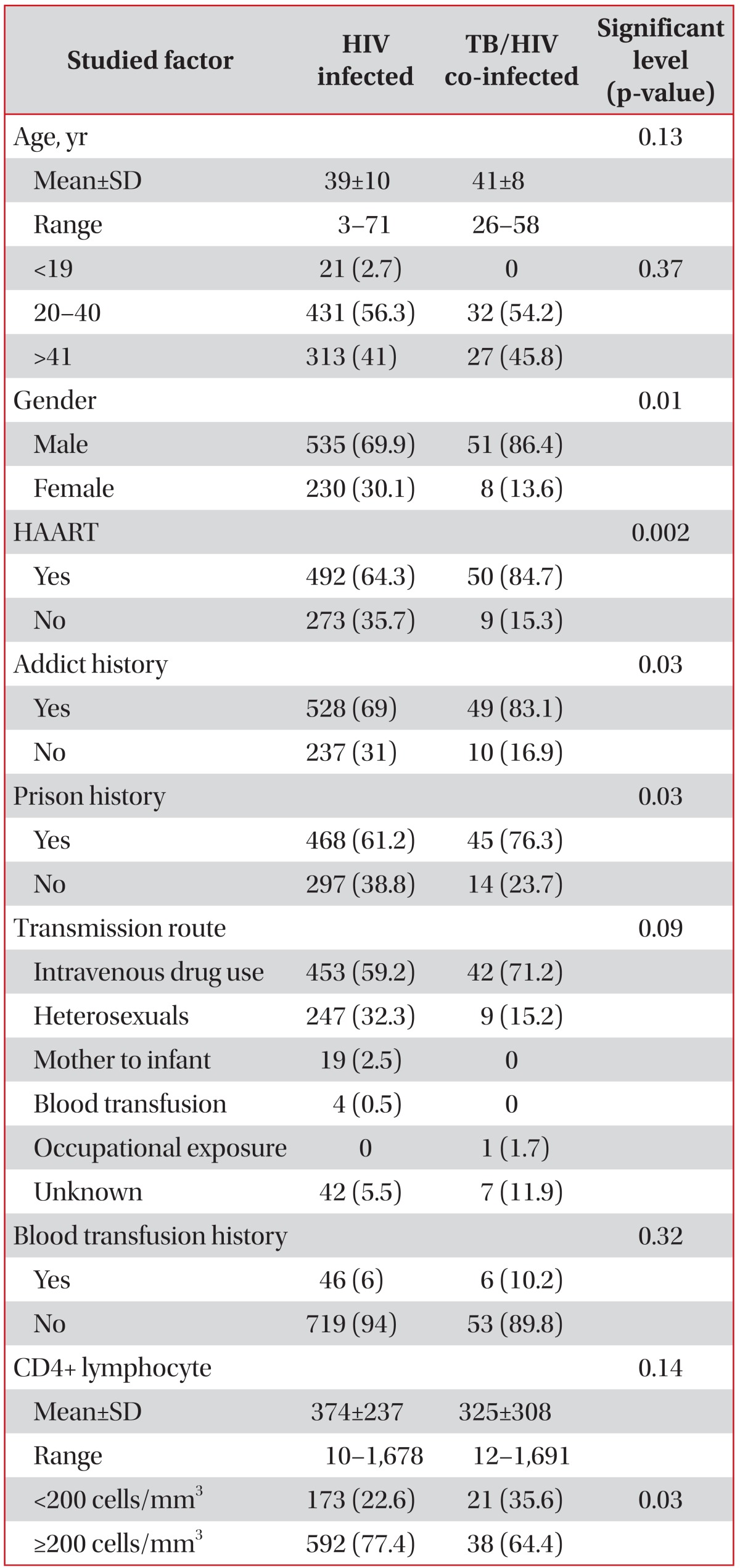
Of 824 HIV infected patients enrolled in this study, 59 (7.2%) were identified as TB co-infected. Although co-infected patients were more likely seen among older patients (the younger case with TB infected was 26 years old), no statistical differences were found among them compared to HIV mono-infected patients. Gender, addiction history, and prison history seems to have a significant risk in developing TB (p<0.05). Also, it seems that frequency of HIV/TB co-infection in our region is more likely among males, since the rate of TB infection was significantly higher among them (p=0.01). The common transmission route in both HIV infected and HIV/TB co-infected patients was intravenous drug use, and transmission routes do not show any significant role in the increased risk of TB infection. Among clinical manifestations, highly active anti-retroviral therapy (HAART) shows a significant difference between the two groups (p=0.002), and the majority (84.7%) of TB infected patients had previously experienced HAART therapy. The full list of demographic and clinical information of both groups is displayed in Table 1.
In our findings, there were associations between co-infection with TB and CD4+ lymphocyte count, since the rates of CD4+ lymphocyte <200 cells/mm3 were significantly (p=0.03) higher among HIV/TB co-infected patients (35.6%) compared to HIV patients (22.6%). The distribution pattern of CD4+ lymphocyte count between HIV infected and HIV/TB co-infected patients is demonstrated in Figure 1.

The distribution pattern of CD4+ lymphocyte count between human immunodeficiency virus (HIV) infected and HIV/tuberculosis (TB) co-infected patients.
Of 59 TB infected cases, the majority of TB clinical forms were pulmonary (73%) followed by lymph nodes (10.2%), pleural (5.1%), and other forms (11.7%). Sputum smears for AFB were positive in 62.8% of pulmonary cases. Of total TB infected cases, chest X-ray abnormalities were seen among 12 patients (20.3%). Thiry-three point three percent of cases with chest X-ray abnormalities and 36.2% of those with normal chest X-ray had CD4+ lymphocyte count <200 cells/mm3; the differences were not significant.
The overall prevalence of MDR is determined 10.2% (n=6) among the all TB co-infected cases. Age and CD4+ lymphocyte count means for MDR cases were 40±5 and 163±166 cells/mm3, respectively.
The mean of CD4+ lymphocyte count and frequency of cases with CD4+ lymphocyte count <200 cells/mm3 among patients with pulmonary TB were 336±355 cells/mm3 and 44.2%, respectively. The lower rates were estimated for patients with extra-pulmonary TB, 295±109 cells/mm3 and 12.5% for CD4+ lymphocyte count mean and frequency of CD4+ lymphocyte count <200 cells/mm3, respectively. However, the observed mean differences between the two groups was not significant (p=0.65).
Discussion
HIV and TB are considered each as a great threat to human life, but confluence of these diseases with each other has deadly consequences12. The morbidity and mortality rate of HIV/TB co-infected patients are several folds higher than mo-no-infected patients with HIV or TB12. However, HIV seems to more likely dedication itself for HIV/TB syndemic, since it has been documented in several studies that the growing HIV epidemic leads to an increase in the rate of TB cases12. Previously, the highly infectious nature of HIV/MDR-TB co-infected patients was noted2. Also, approximately more than 30% of TB related deaths among co-infected patients belonged to MDR-TB12. These facts highlight the importance of early detection and treatment of HIV/MDR-TB co-infected patients. To best of our knowledge, the present study reports for first time the prevalence of MDR-TB to be 10.2% among HIV patients in Iran. Despite the lack of data on prevalence of MDR-TB among HIV patients in Iran, previously reports of MDR-TB among non-HIV patients shown lower rates compared to our results and highest ever seen prevalence was up to 9%78910111213. It seems that HIV/TB co-infected patients had more chance to develop MDR-TB than non-HIV patients; however, more studies needs for other parts of our country to reach an overall conclusion.
In the findings of our study, the rate of HIV/TB co-infection was 7.2%. This rate could be affected by several social and clinical factors. However, Wondimeneh et al.14 from northwest Ethiopia is closer to our results, reporting the rate of HIV/TB co-infection to be 7.5%; Rabirad et al.15 from capital of Iran reported 28.2% for this rate which was notably higher than our findings. However, it can be the consequence of lower CD4+ lymphocyte count in Rabirad et al.'s study15 compared to ours, 144 cells/mm3 versus 325 cells/mm3, respectively. Moreover, in our study the majority (84.7%) of co-infected patients experienced HAART therapy. The rate of HIV/TB co-infection also had a close correlation with the incidence of TB, so the varied rates form different parts of the world with different TB incidences are not surprising161718192021.
TB co-infection in our patients was more likely seen among men; this pattern is shown in most of the similar studies around the world161822. Almost half of our HIV infected and TB co-infected patients were young adults (21-40 years old); previously, in agreement with our results several studies demonstrated the predominance of HIV/TB infections among young adults141622. However, it seems to be more logical if we pay attention to the main transmission routes of infections in the present study which were intravenous drug use and heterosexuality. Logically, a lower chance for these transmission routes account among individuals younger than the teen age. Some social determinants may influence the hosts' susceptibility to TB infection; among these risk factors poor ventilation, overcrowding, poverty and malnutrition could be mentioned2324. In the current study, addiction and prison history cause a significant risk in developing TB. The enclosed settings, such as prisons, can increase the risk of TB infection because of poor infection control and ventilation12.
The association between levels of CD4+ lymphocyte and prevalence of TB among HIV related immune-suppressed patients has been demonstrated in several studies142526. In the present study, the mean of CD4+ lymphocyte count for HIV/TB co-infected patients was lower than that of HIV infected patients (325 cells/mm3 vs. 374 cells/mm3, respectively). In addition, frequency of CD4+ lymphocyte count less than 200 cells/mm3 was higher among TB infected patients and this difference was statistically significant.
One of the important roles of CD4+ T cells in developing TB is generation of granuloma36. The decreased CD4+ cells level in patients with advanced HIV increased the risk TB infection dissemination and subsequently chance of extra-pulmonary312. In our results, patients with extra-pulmonary TB had lower CD4+ lymphocyte counts (295 cells/mm3) than those suffering from puflmonary TB (336 cells/mm3). The rate of extra-pulmonary infections among our TB infected patients was 27%; this rate are shown very varied when compared to other studies around the world, such as Brazil (36.6%), Russia (28%), Korea (19%), and Iran (14%)18202127. In contrast with other studies that stated patients with higher CD4+ cells are more likely to have chest X-ray abnormalities, no evidence was found in our results to confirm this hypothesis2829.
In conclusion, we report unique information on prevalence of HIV/TB co-infection and also MDR-TB outcome among co-infected patients. One of the most important tools in infection control programs, especially for specific situations such as HIV/TB co-infection, is having a general vision to the current conditions and the related factors associated with infections outcome. Such surveillance studies could provide useful insights for better management, not only at the regional level but also at the global scale.
Acknowledgements
We thank all the participants for their friendly cooperation in this study. This work was supported by the Shiraz HIV/AIDS Research Center, Shiraz University of Medical sciences, Iran.
Notes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.