Snoring during Bronchoscopy with Moderate Sedation Is a Predictor of Obstructive Sleep Apnea
Article information
Abstract
Background
Snoring is the cardinal symptom of obstructive sleep apnea (OSA). Snoring and upper airway obstruction associated with major oxygen desaturation may occur in populations undergoing flexible bronchoscopy.
Methods
To evaluate the prevalence of patients at a high risk of having OSA among patients undergoing bronchoscopy with sedation and to investigate whether snoring during the procedure predicts patients who are at risk of OSA, we prospectively enrolled 517 consecutive patients who underwent the procedure with moderate sedation. Patients exhibiting audible snoring for any duration during the procedure were considered snorers. The STOP-Bang (Snoring, Tiredness, Observed apnea, high blood Pressure-Body mass index, Age, Neck circumference and Gender) questionnaire was used to identify patients at high (score ≥3 out of 8) or low risk (score <3) of OSA.
Results
Of the 517 patients, 165 (31.9%) snored during bronchoscopy under sedation. The prevalence of a STOP-Bang score ≥3 was 61.9% (320/517), whereas 200 of the 352 nonsnorers (56.8%) and 120 of the 165 snorers (72.7%) had a STOP-Bang score ≥3 (p=0.001). In multivariable analysis, snoring during bronchoscopy was significantly associated with a STOP-Bang score ≥3 after adjustment for the presence of diabetes mellitus, chronic obstructive pulmonary disease, chronic kidney disease, and stroke (adjusted odds ratio, 1.91; 95% confidence interval, 1.26–2.89; p=0.002).
Conclusion
Two-thirds of patients undergoing bronchoscopy with moderate sedation were at risk of OSA based on the screening questionnaire. Snoring during bronchoscopy was highly predictive of patients at high risk of OSA.
Introduction
Obstructive sleep apnea (OSA) is recognized as the occurrence of repetitive episodes of partial airway collapse, manifested as loud snoring and hypopnea, or complete airway collapse, manifested as apnea, which results in oxygen desaturation or arousal during sleep. In the 1990s, the prevalence of OSA was 4% in middle-aged men and 2% in middle-aged women1. However, the prevalence of OSA has increased substantially over the past two decades, ranging from 10% to 20%, with the increasing prevalence of obesity and advanced age23. OSA is frequently comorbid with cardiovascular, cerebrovascular, and metabolic diseases4, and is responsible for poor quality of life and increased health care use costs5. Furthermore, OSA is associated with high morbidity and mortality rates67.
However, OSA remains underdiagnosed; up to 80% of patients with moderate to severe OSA are estimated to remain undiagnosed in the general population8. Even in surgical patients, approximately 60% of those with moderate to severe OSA are not recognized preoperatively910. Thus, efforts have been made to devise simple screening instruments to identify patients who are undiagnosed but at high risk of OSA because overnight polysomnography is time-consuming, labor-intensive, and costly11121314.
Snoring is the cardinal symptom of OSA. Both male and female habitual snorers are more likely to have an apnea-hypopnea index (AHI) of 15 or higher1. By contrast, the absence of snoring makes OSA less likely4.
Although flexible bronchoscopy is a generally safe and minimally invasive diagnostic procedure, patients with OSA may have an increased risk of obstructive episodes during procedures with moderate sedation15. Snoring and upper airway obstruction associated with oxygen desaturation have been reported to occur in patients undergoing bronchoscopy16. However, the association between snoring during bronchoscopy and OSA remains largely unexplored. Here, we aimed to evaluate the prevalence of patients at a high risk of having OSA in a population undergoing bronchoscopy with moderate sedation and to investigate whether snoring during the procedure predicts patients who are at risk of OSA. Detecting additional clinical predictors of OSA may help identify patients for whom further evaluation of OSA is necessary.
Materials and Methods
1. Study design and patients
We prospectively enrolled consecutive patients who were 18 years or older and undergoing flexible bronchoscopy with moderate sedation in the bronchoscopy center at Seoul National University Hospital between 27 December 2016 and 1 October 2018. Patients were excluded from the study if they had a previous diagnosis of OSA, an American Society of Anesthesiologists physical status >3, or baseline pulse oximeter oxygen saturation (SpO2) <90%, or used a tracheostomy tube, needed supplemental oxygen before the procedure, or had been scheduled to undergo bronchoalveolar lavage, endobronchial ultrasound-guided transbronchial needle aspiration, or interventional bronchoscopy.
This study was approved by the Institutional Review Board of Seoul National University Hospital (H-1612-041-813). All participants provided written informed consent and the study was conducted in accordance with the tenets of the Declaration of Helsinki.
2. Screening for OSA
The STOP-Bang (Snoring, Tiredness, Observed apnea, high blood Pressure-Body mass index, Age, Neck circumference and Gender) questionnaire was adopted as a screening tool for OSA in the present study11. The STOP-Bang questionnaire was developed and validated to identify patients with undiagnosed OSA in preoperative clinics. The questionnaire comprises eight yes-or-no questions (snoring, tiredness, observed apnea, high blood pressure, body mass index [BMI] >35 kg/m2, age >50 years, neck circumference >40 cm, and male sex). It has a high sensitivity at a cutoff score of ≥3: 84% in detecting any OSA (AHI >5/hr) and 93% in detecting moderate to severe OSA (AHI >30/hr)11. A recent study proposed an alternative model for scoring the STOP-Bang questionnaire to improve the specificity for detecting moderate to severe OSA1718. According to the alternative model, participants are classified into three groups based on the STOP-Bang score: low (0–2), intermediate (3–4), and high risk (5–8). Those with STOP-Bang scores of 3 or 4 can be further classified as having a high risk of moderate to severe OSA if they have both a STOP (snoring, tiredness, observed apnea, high blood pressure) score of ≥2 and meet one of the following criteria: (1) BMI >35 kg/m2, (2) neck circumference >40 cm, or (3) male sex1718. The results of the questionnaire were not disclosed to the attending nurses and bronchoscopists.
3. Sedation and monitoring
Our routine practice for flexible bronchoscopy is to use moderate sedation with intravenous midazolam. Midazolam was administered by an experienced nurse and titrated by the attending bronchoscopist. If required, 50 µg of fentanyl as an adjuvant was infused at the bronchoscopist's discretion. From the onset of sedation, all patients were provided with 3 L/min of supplemental oxygen by nasal cannula with continuous pulse oximetry and electrocardiography, and intermittent blood pressure monitoring. Snoring during bronchoscopy was also monitored. Patients exhibiting audible snoring for any duration during the procedure were considered snorers in this study.
4. Statistical analysis
Clinical characteristics were compared between snorers and nonsnorers using the independent samples t test for continuous variables. Categorical variables were compared using either the chi-square test or Fisher exact test. Multivariable logistic regression was performed to evaluate the association of snoring during bronchoscopy with a STOP-Bang score ≥3 adjusted for variables with p-values of <0.05 in univariable analysis considering collinearity.
A p-value of less than 0.05 was considered significant. Statistical analyses were performed using Stata statistical software (version 13.1, StataCorp LP, College Station, TX, USA).
Results
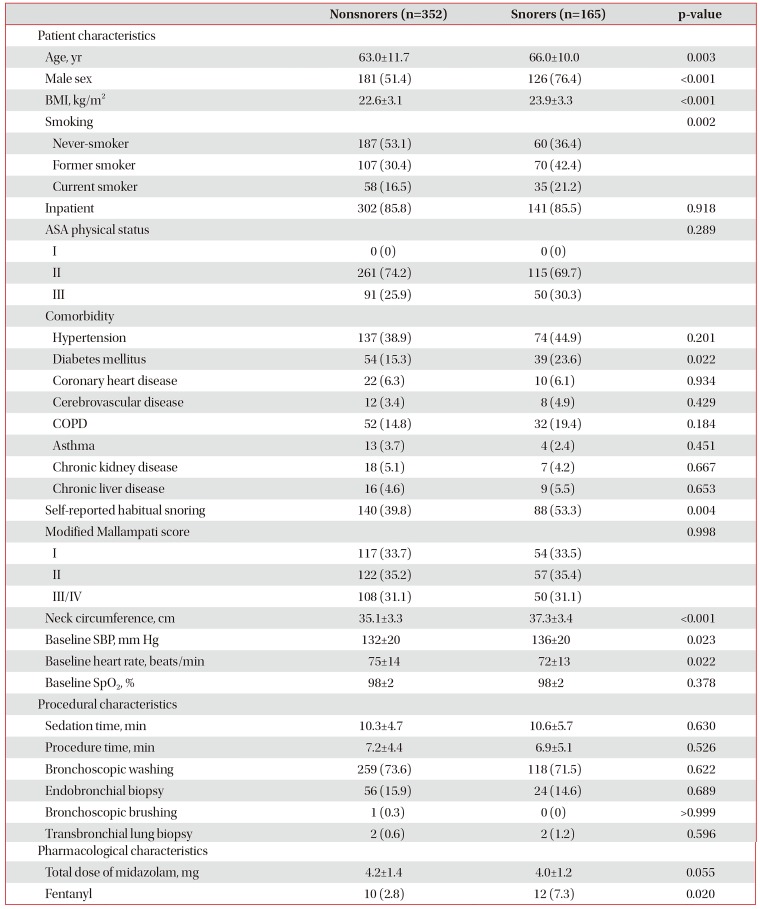
Among the 544 patients who were enrolled during the study period, 27 were excluded from the analysis because of incomplete documentation. Of the 517 included patients, 165 (31.9%) snored during bronchoscopy under moderate sedation. Table 1 summarizes patient, procedural, and pharmacological characteristics. Snorers were significantly older and predominantly male compared with nonsnorers. Snorers had a higher BMI and neck circumference than nonsnorers. Snorers were more likely to be ever-smokers and have comorbid diabetes mellitus. Although patients who snored during the procedure were more likely to report habitual snoring, approximately half of snorers did not report habitual snoring, whereas nearly 40% of nonsnorers reported habitual snoring. The modified Mallampati score was similar in both snorers and nonsnorers. The mean dose of midazolam did not differ significantly between the groups, but the use of fentanyl was more frequent in snorers.
The prevalence of a STOP-Bang score ≥3 was 61.9% (320/517), whereas 200 of the 352 nonsnorers (56.8%) and 120 of the 165 snorers (72.7%) had a STOP-Bang score ≥3 (p=0.001). When the alternative scoring model of the STOP-Bang questionnaire was used, 42.4% of snorers and 24.2% of nonsnorers were classified as having a high risk of moderate to severe OSA (Figure 1).

Proportion of snorers and nonsnorers with low, intermediate, and high risk of obstructive STOP-Bang (Snoring, Tiredness, Observed apnea, high blood Pressure-Body mass index, Age, Neck circumference and Gender) questionnaire.
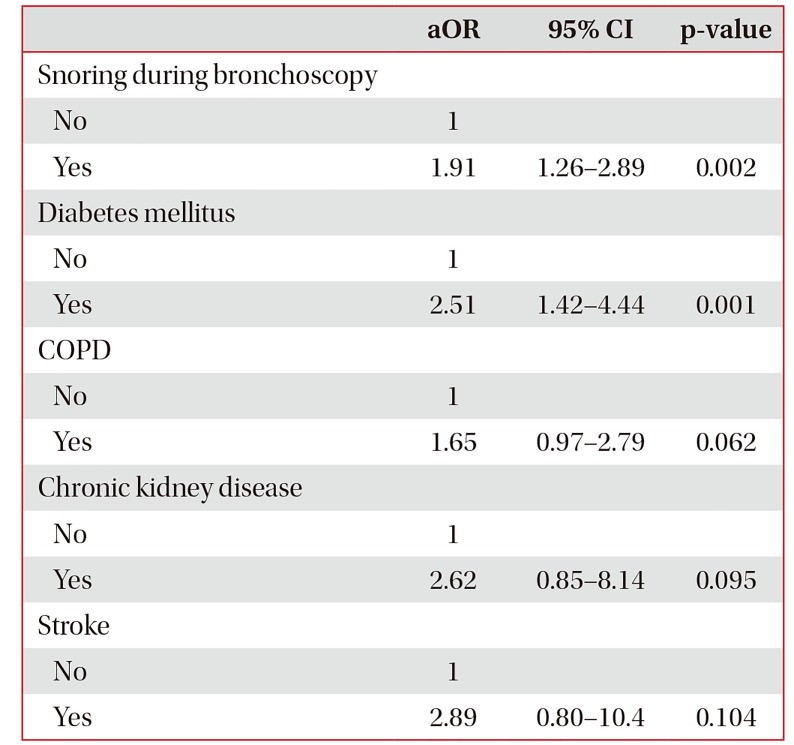
In multivariable analysis, snoring during bronchoscopy was significantly associated with a STOP-Bang score ≥3 after adjustment for the presence of diabetes mellitus, chronic obstructive pulmonary disease, chronic kidney disease, and stroke (adjusted odds ratio, 1.91; 95% confidence interval, 1.26–2.89; p=0.002) (Table 2).
Discussion
In the present study, we found that two-thirds of patients undergoing bronchoscopy with moderate sedation were at risk of OSA based on the screening questionnaire. A third of patients snored during the procedure. Snoring during bronchoscopy predicted patients who were at risk of OSA after adjustment for comorbidities.
Snoring is a sleep-related sound caused by vibration of the soft tissue in the upper airway under conditions of inspiratory airflow limitation4. Snoring is generated by high-frequency opening and closing of the upper airway structures, including the tongue base and soft palate, aided by the adhesive properties of mucosal secretions4. The associations of snoring with hypertension, myocardial infarction, and stroke were reported in the early 1990s19202122, and habitual snorers were found to be more likely to have moderate to severe OSA in the general population1. Recently, the amount of time spent snoring was demonstrated to be correlated with the extent of asymptomatic carotid artery stenosis23.
Intravenous sedation should be provided to patients undergoing flexible bronchoscopy, particularly when no contraindications to sedation are present24. Intravenous midazolam is the preferred sedative for bronchoscopy because of its relatively rapid onset of action and short half-life compared with those of other benzodiazepines. Midazolam induces central nervous system depression, partially by increasing the activity of γ-aminobutyric acid, the major inhibitory neurotransmitter in the brain25, while also increasing upper airway resistance leading to obstructive apnea26. Moreover, when patients undergo bronchoscopy in the supine position, they may have a higher risk of upper airway collapse than patients who undergo gastrointestinal endoscopy in the left lateral decubitus position.
Studies evaluating the risk of OSA in patients undergoing bronchoscopy with moderate sedation are scarce, but it has been reported that approximately 40% of patients undergoing routine and advanced gastrointestinal endoscopy are at risk of OSA152728. In our study regarding flexible bronchoscopy, approximately 60% of patients were at risk of OSA.
Sharara et al.29 reported that persistent snoring under moderate sedation during colonoscopy was a strong predictor of OSA, which was confirmed by out-of-center sleep testing. However, in their study, participants who had major comorbidities and underwent the procedure on an inpatient basis were excluded. By contrast, we enrolled both inpatients and outpatients regardless of comorbidities. In this unselected cohort, snoring during bronchoscopy was significantly associated with the risk of OSA after adjustment for the comorbidities frequently associated with OSA.
Patients with OSA may experience adverse events during procedures with sedation15. However, adverse events in undiagnosed OSA patients undergoing bronchoscopy with moderate sedation remain poorly recognized. Previous studies on the risk of adverse events have focused on populations undergoing gastrointestinal endoscopy. Patients at high risk of OSA had increased cardiopulmonary events when they underwent advanced endoscopic procedures such as endoscopic retrograde cholangiopancreatography and endoscopic ultrasound15 but not when they underwent routine esophagogastroduodenoscopy and colonoscopy2728303132. Differences in the duration and depth of sedation as well as in patient positioning during procedures may account for the different rates of cardiopulmonary events. Although flexible bronchoscopy is a minimally invasive diagnostic procedure, it is generally considered to have a greater risk of cardiopulmonary events than gastrointestinal endoscopy. Consequently, further investigation is warranted to evaluate cardiopulmonary events in patients undergoing bronchoscopy with moderate sedation.
To appreciate the results of our study appropriately, we have to recognize its limitations. First, we were unable to confirm the diagnosis of OSA using polysomnography in patients with a STOP-Bang score ≥3. However, the STOP-Bang questionnaire has been validated and its high sensitivity in detecting moderate to severe OSA has been documented repeatedly18. Second, capnography monitoring was not applied; although capnography detects episodes of apnea or hypoventilation, it is not widely used in routine practice.
In conclusion, we found that undiagnosed OSA, estimated using a screening questionnaire, was prevalent in patients undergoing bronchoscopy with moderate sedation. Snoring during bronchoscopy was highly predictive of patients at high risk of OSA. Snoring during the procedure may help uncover undiagnosed OSA and triage patients who need referral for polysomnography.
Notes
Authors' Contributions:
Conceptualization: Lee J, Cho J.
Methodology: Lee J, Cho J.
Formal analysis: Cho J.
Investigation: Lee J, Cho J, Choi SM, Park YS, Lee CH, Lee SM.
Writing - original draft preparation: Lee J, Cho J.
Writing - review and editing: Lee J, Cho J.
Approval of final manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
Funding: No funding to declare.