Revised (2018) COPD Clinical Practice Guideline of the Korean Academy of Tuberculosis and Respiratory Disease: A Summary
Article information
Abstract
Chronic obstructive pulmonary disease (COPD) results in high morbidity and mortality among patients nationally and globally. The Korean clinical practice guideline for COPD was revised in 2018. The guideline was drafted by the members of the Korean Academy of Tuberculosis and Respiratory Diseases as well as the participating members of the Health Insurance Review and Assessment Service, Korean Physicians' Association, and Korea Respiration Trouble Association. The revised guideline encompasses a wide range of topics, including the epidemiology, diagnosis, assessment, monitoring, management, exacerbation, and comorbidities of COPD in Korea. We performed systematic reviews assisted by an expert in meta-analysis to draft a guideline on COPD management. We expect this guideline to facilitate the treatment of patients with respiratory conditions by physicians as well other health care professionals and government personnel in South Korea.
Introduction
According to a survey conducted by the Korean Academy of Tuberculosis and Respiratory Diseases in 2008, people over the age of 40 years have a high chronic obstructive pulmonary disease (COPD) prevalence rate of 13%1. The trends in the prevalence of COPD in Korea using the data from Korea National Health and Nutrition Examination Survey (KNHANES) did not change much, which ranged from 13.1% to 14.6% during the period from 2010 to 20152. According to the National Statistical Office, COPD is one of the 10 major causes of death in South Korea3. The World Health Organization (WHO) expects that the prevalence and mortality rates of COPD will increase worldwide4. The WHO also emphasizes the importance of prevention, early diagnosis, and proper treatment of COPD by selecting it as one of the five noninfectious diseases that must be managed worldwide. In 2012 and 2014, the Korean Academy of Tuberculosis and Respiratory Diseases published the COPD clinical practice guideline (in Korean and summary 2014 revised version in English), which could be used in clinical practice. In 2018, the revised version of the COPD guideline (in Korean) was published on the basis of the findings of new studies published over the previous 4 years. This revision has been made not only by the Korean Academy of Tuberculosis and Respiratory Diseases but also by the Health Insurance Review and Assessment Service, Korean Physicians' Association, and Korea Respiration Trouble Association. Therefore, the revised clinical practice guideline is more advanced than the original one. We expect this guideline would be helpful not only to medical doctors treating patients with respiratory conditions but also to other health care professionals and government personnel in South Korea.
Definition, Epidemiology, Cause, and Mechanism
COPD can be defined as follows.
“It is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by smoking, occupational exposure, indoor air contamination, and infection.” As it is a very common disease, it has a severe socioeconomic influence. Acute exacerbation occurs frequently and comorbid diseases are comparatively more common in the general population, influencing the severity and prognosis of COPD.
COPD is a leading cause of morbidity and mortality worldwide45. The prevalence of COPD has increased over the decades. This phenomenon is due to consistent exposure to COPD risk factors and global population aging, and it is anticipated to continue into the future. A study by the WHO estimated that in 2007, the global number of patients with COPD was 210 million6, but other large epidemiologic such as Burden of Obstructive Lung Disease estimated that in 2010, number COPD patient was 380 million and prevalence was 11.7% worldwide7. As for the COPD prevalence in Korea, 13.4% of the population over 40 years of age has COPD based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria (forced expiratory volume in 1 second/forced vital capacity [FEV1/FVC] <0.7), with 21.6% of the male population and 5.8% of the female population having COPD based on the 2015 KNHANES2. The COPD prevalcence is unchanged for 7 years in Korea. However, among patients diagnosed with COPD, only 2.8% were diagnosed with COPD by a doctor, and only 1.6% received treatment. This suggests that most Korean patients with COPD are not diagnosed and treated. COPD is an important cause of mortality in most countries. According to the Global Burden of Disease Study conducted in 1990, COPD ranked sixth among the global causes of death, but it is anticipated to rank third in 2020 and fourth in 20304. According to Statistics Korea, the total number of deaths from COPD, based on disease code, was 3,329 in the year 2000 (2,120 among men and 1,209 among women), and 5,002 in the year 2010 (3,526 among men and 1,476 among women). In 2015, chronic lower airway disease ranked seventh among the overall causes of death, accounting for a total of 7,538 deaths. In an aging population, the risk of death from COPD has been increasing, and it ranks fifth among the overall causes of death in the age group of 80 years or older, with a mortality rate of 3,732 per 100 thousand3.
Additionally, COPD results in a huge socioeconomic burden. In Korea, based on the 2010 data of the Health Insurance Review and Assessment Service, about 284 billion Korean Won is spent on the medical treatment of COPD. According to the 2009 data of the Health Insurance Review and Assessment Service, the medical fee per individual is as high as 3.23 million Won, and it has been increasing rapidly in recent years8. Moreover, in 1990, COPD ranked 12th among the cause of disability-adjusted life years (DALYs) loss in the world, but it is anticipated to rank seventh in 20304. In Korea, DALYs from COPD have rapidly increased from 270 years per 100 thousand in 2002 (ranking 10th) to 550 years per 100 thousand in 2007 (ranking seventh). Accodrding to 2012 Korean Burden of Disease Study, DALY from COPD is 1,305 years per 100 thousand and it occupies 6.21% of DLAY lost caused by non-communicable disease9.
The most important and well-known risk factor for COPD is smoking. Other risk factors include occupational dust, chemical materials, air pollution, low socioeconomic status, chronic bronchitis, and respiratory infection. Host factors related to COPD include genetics, age, sex, lung growth, and airway hypersensitivity1011. Smoke and harmful substances induce lung inflammation, and lung parenchyma damage from such inflammation and disruption of the normal repair system can induce emphysema and small airway fibrosis12. Such pathologic alteration induces air trapping and airflow limitation.
Diagnosis and Assessment
A person over the age of 40 years exposed to cigarette smoke or other risk factors and showing symptoms of dyspnea, cough, and sputum production should be suspected of having COPD13.
To diagnose COPD, a patient should undergo spirometry that determines the FEV1, FVC, and the ratio of FEV1/FVC. FEV1/FVC <0.7 confirms an airflow limitation, which is an objective diagnostic evidence of COPD. More importantly, spirometry should be performed after short-acting bronchodilator inhalation to confirm the airflow limitation in COPD.
For COPD treatment, spirometry, symptom grade, and exacerbation history should be assessed. First, the severity of COPD on spirometry should be classified into two categories: FEV1 ≥60% vs. FEV1 <60%. Second, the symptom grade should also be classified into two categories: the modified Medical Research Council dyspnea scores (mMRC) 0–1 vs. mMRC ≥2, or the score of the COPD assessment test score (CAT) <10 versus CAT ≥10. Third, the exacerbation frequency should be classified as follows: 0–1/yr vs. ≥2/yr. According to this assessment, patients with COPD are classified into three groups: Ga, Na, and Da (Figure 1). When patients with COPD show other accompanying diseases, such as cardiovascular disorders, osteoporosis, depression, or lung cancer, their prognosis is poor. Therefore, the comorbid diseases accompanying COPD should be evaluated.
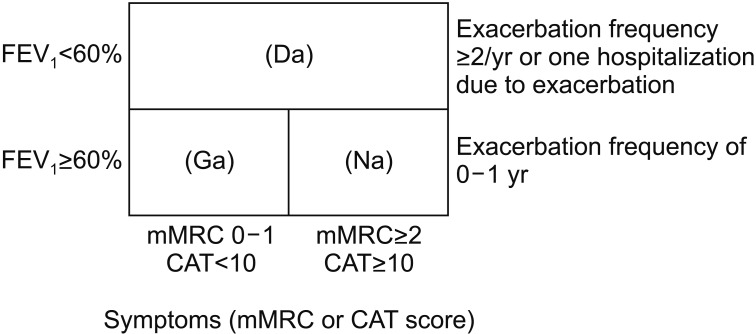
Classification of patients with chronic obstructive pulmonary disease (COPD). FEV1: forced expiratory volume in 1 second; mMRC: modified Medical Research Council dyspnea score; CAT: COPD assessment test score.
Patients with asthma-COPD overlap syndrome exhibit features of both asthma and COPD. Experts suggest that treatment for both asthma and COPD should be administered to such patients.
An mMRC dyspnea grade of 2 refers to the situation where a patient walks slower on ground level than a similarly aged person because of shortness of breath, or when a patient stops for breathing when walking at his or her own pace on ground level.
FEV1 of 50% predicted value, the previous cut-off threshold has been deleted in the GOLD 2017 documents. However, we decide to maintain the previous FEV1 cut-off threshold of 60% predicted value because spirometry needs to be performed more in most of the primary care clinics in Korea and also because only spirometry value is objective measurements while dyspnea score and exacerbation frequency are subjective.
We have defined the Da group which is an analogy of the combination, both GOLD group C and D. As for the GOLD group C, the proportion of it is very small in a clinical practice setting and the recommended medications are similar to those of the GOLD group D. So we decided the combined group, Da.
In conclusion, we decide not to change the frame of combined assessment in the Korean COPD guideline revised in 2014. So, the contents of diagnosis and assessment are quite same in the Korean COPD guidelines revised both in 2014 and 2018.
Management of Stable COPD
The goals of management of stable COPD are to reduce both current symptoms and future risks with minimal side effects from treatment. Ongoing monitoring should ensure that the treatment goals are being met, and it should include continuous evaluation of exposure to risk factors and monitoring of disease progression, the effect of treatment and possible adverse effects, exacerbation history, and comorbidities. Identification and reduction of exposure to risk factors are important in the treatment and prevention of COPD.
1. Pharmacologic management
Appropriate pharmacologic therapy can reduce symptoms, reduce the frequency and severity of exacerbations, and improve health status and exercise tolerance. To date, none of the existing medications for COPD has been shown to modify disease progression or reduce mortality14,15,16.
1) Bronchodilators
Bronchodilators are the cornerstone of pharmacological treatment in COPD (Table 1). Inhalation therapy is preferred over oral, subcutaneous, or intravenous administration, because inhalation therapy can maximize the bronchodilator's effect on the airway with least systemic side effects. When treatment is administered via inhalation, attention is essential to ensure effective drug delivery and training in inhaler technique. A metered-dose inhaler, dry powder inhaler, soft mist inhaler, or nebulizer can be used for inhalation therapy, according to the patient's clinical situation.
(1) β2-agonists: Short-acting β2-agonists (SABAs) are recommended as needed for the relief of dyspnea and exercise limitation17. Many trials have proven the clinical benefits of long-acting β2-agonists (LABAs) in COPD, including the improvement of health status, FEV1, FVC, and exercise capacity. Therefore, regular treatment with LABAs is more highly recommended than irregular usage of SABAs on an as-needed basis to address the airflow limitation in COPD. Indacaterol is a once daily β2-agonist with duration of action of 24 hours. This bronchodilator's effect is significantly greater than that of formoterol and salmeterol, and similar to that of tiotropium. Indacaterol has significant effects on breathlessness and health status1819.
(2) Anticholinergic agents: Long-acting muscarinic agents (LAMAs) provide clinically significant improvements in lung function, reduce acute exacerbation, and improve health status and the effects of pulmonary rehabilitation in patients with COPD2021. A large, long-term clinical trial on patients with COPD showed no effect of tiotropium added to other standard therapies on the rate of lung function decline and no evidence of cardiovascular risk22. Clinical trials have shown a greater effect on exacerbation rates for LAMA treatment (tiotropium) versus LABA (indacaterol, salmeterol) treatment2324. The long-acting anticholinergics aclidinium2526272829 and glycopyrronium303132 seem to have a similar action as tiotropium on lung function and breathlessness; however, far less data are available for other outcomes.
(3) Methylxanthines: Methylxanthines may act as nonselective phosphodiesterase inhibitors, but they have also been reported to have a range of nonbronchodilator actions, whose significance has been disputed. Theophylline is the most commonly used methylxanthine. Theophylline is less effective and less well tolerated than inhaled long-acting bronchodilators, and it is not recommended if the latter drugs are available and affordable. The addition of theophylline to salmeterol produced a greater improvement in FEV1 and breathlessness than did salmeterol alone33. Low-dose theophylline reduces exacerbations but does not improve postbronchodilator lung function.
(4) Combination bronchodilator therapy: Combining bronchodilators with different mechanisms and durations of action may increase the degree of bronchodilation with equivalent or lesser side effects. There are several combinations of a LABA and LAMA in a single inhaler available. These combinations have shown a significant improvement in dyspnea, health status and lung function as well as a prevention of exacerbation compared with that shown by monotherapy3435. Combinations of a LABA and LAMA showed not only noninferiority but also consistent superiority to the inhaled steroid and LABA combination for outcomes related to exacerbation, lung function, and health status36.
2) Corticosteroids
(1) Inhaled corticosteroids: Most studies have found that regular treatment with inhaled corticosteroid (ICS) alone does not modify the long-term decline of FEV1 nor mortality in patients with COPD14163738.
(2) Combination of ICSs and long-acting bronchodilators: An ICS combined with a LABA is more effective than the individual components in improving lung function and health status and reducing exacerbations in patients with moderate to very severe COPD3940. However, a large, prospective clinical trial failed to demonstrate a statistically significant effect of combination therapy on mortality37. Moreover, combination therapy is associated with an increased risk of pneumonia. Post-hoc analysis from several trials and observation studies suggest that eosinophil counts in sputum and blood and asthma COPD overlap may serve as parameter to predict the efficacy of ICS in particular regarding exacerbation prevention. Triple therapy of ICS/LABA/LAMA had clinical benefits compared with tiotropium or ICS/LABA combination with symptomatic COPD and a history of exacerbations in a reduction in the rate of exacerbation and improvement in lung function414243.
3) Phosphodiesterase-4 inhibitors
Roflumilast is suggested for patients with COPD with severe airflow limitation (postbronchodilator FEV1/FVC, 0.7; FEV1 <50%), symptoms of chronic bronchitis, and a history of exacerbations, in whom the disease is not adequately controlled by long-acting bronchodilators44454647484950 or fixed dose ICS/LABA5152. The beneficial effects of roflumilast have been reported to be greater in patients with a prior history of hospitalization for an acute exacerbation. The most frequent adverse effects are nausea, reduced appetite, weight loss, abdominal pain, diarrhea, sleep disturbances, and headache44454647.
4) Other pharmacologic treatments
(1) Vaccination: Influenza vaccination and pneumococcal vaccination are recommended for patients with COPD.
(2) Antibiotics: Although studies have shown some effects of antibiotics on exacerbation rate53545556, the role of this treatment is unclear. Prophylactic antibiotic treatment is not recommended because of an unfavorable balance between the benefits and side effects.
2. Pharmacologic treatment algorithms based on the Korean COPD classification (Figure 2)
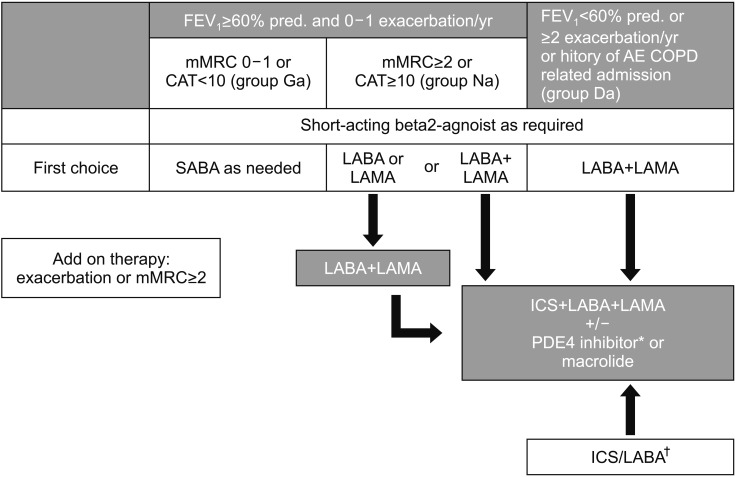
Pharmacologic treatment algorithms. *Postbronchodilator FEV1 <50%, symptoms of chronic bronchitis, and a history of exacerbations. †Asthma overlap or high blood eosinophil. COPD: chronic obstructive pulmonary disease; FEV1: forced expiratory volume in 1 second; mMRC: modified Medical Research Council dyspnea score; CAT: COPD assessment test score; AE COPD: acute exacerbation of COPD; SABA: short-acting β2-agonists; LABA: long-acting β2-agonists; LAMA: long-acting muscarinic antagonist; PDE4: phosphodiesterase-4; ICS: inhaled corticosteroid.
1) Group Ga patients
SABA is recommended as a first-line therapy since SABA can improve lung function and decrease dyspnea. If dyspnea (mMRC ≥2) or acute exacerbation develops despite medical treatment, LABA or LAMA can be tried. However, not enough trials have been conducted on group Ga COPD.
2) Group Na patients
LABA or LAMA is recommended as a first-line therapy. Randomized controlled trials comparing LABA and LAMA have shown no significant difference in the outcomes such as pulmonary function, symptomatic improvement, and health status. The choice of long-acting bronchodilators should depend on the patient's perception of symptom relief, side effects, and clinician's discretion. For patients with severe breathlessness, the alternative is a combination of long-acting bronchodilators. Combination therapy with LAMA and LABA can be provided for patients who show no improvement of symptoms with single therapy or undergo frequent exacerbation.
3) Group Da patients
Combination therapy with LABA+LAMA can be administered as a first-line therapy. If patients have asthma or high blood eosinophil, ICS/LABA can be considered as a first-line therapy. If dyspnea (mMRC ≥2) or acute exacerbation develops despite first-line treatment, triple therapy with ICS/LABA/LAMA or addition of a phosphodiesterase-4 (PDE4) inhibitor can be tried. Triple therapy of ICS/LABA/LAMA had clinical benefits compared with tiotropium or ICS/LABA combination with symptomatic COPD and a history of exacerbations in a reduction in the rate of exacerbation and improvement in lung function. PDE4 inhibitors can be administered to this group of patients with COPD and chronic bronchitis phenotype who undergo frequent exacerbations, if the side effects of PDE4 inhibitors, including nausea, diarrhea, and weight loss, are not serious.
3. Nonpharmacologic therapies
1) Smoking cessation
Smoking cessation is one of the most important interventions. It slows the rate of decline in FEV1 with consequent benefits in terms of progression of symptoms and survival57. Pharmacotherapy and nicotine replacement reliably increase the long-term smoking abstinence rates.
2) Physical activity/Pulmonary rehabilitation
The principal goals of pulmonary rehabilitation are to reduce symptoms, improve quality of life, and increase physical and emotional participation in everyday activities58. All patients who experience shortness of breath when walking on their own pace on level ground should be offered rehabilitation. Several studies have documented an effect of pulmonary rehabilitation in patients with breathlessness, usually mMRC >1, and following acute exacerbations.
3) Oxygen therapy
The long-term administration of oxygen (>15 hr/day) to patients with chronic respiratory failure has been shown to increase survival in patients with severe resting hypoxemia59. Long-term oxygen therapy is indicated for patients who have the following conditions:
Partial pressure of oxygen (PaO2) at or below 55 mm Hg or arterial oxygen saturation (SaO2) at or below 88%, with or without hypercapnia confirmed twice over a 3-week period; or PaO2 between 55 mm Hg and 60 mm Hg, or SaO2 of 89%, if there is evidence of pulmonary hypertension, peripheral edema suggesting congestive cardiac failure, or polycythemia (hematocrit >55%).
4) Bronchoscopic lung volume reduction
In a post-hoc analysis, bronchoscopic lung volume reduction (BLVR) in patients with COPD and severe airflow limitation (FEV1, 15–45% predicted), heterogeneous emphysema on computed tomography (CT), and hyperinflation (total lung capacity >100% and residual volume >150% predicted) induced modest improvements in lung function, exercise tolerance, and symptoms, at the cost of more frequent exacerbations of COPD, pneumonia, and hemoptysis after implantation60. Additional data are required to define the optimal BLVR technique and patient population.
Acute Exacerbation of COPD
1. Definition
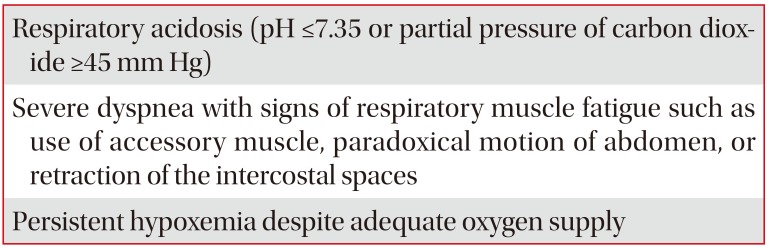
Acute exacerbation of COPD can be defined as episodes of acute worsening of the patient's respiratory symptoms, particularly dyspnea, cough and sputum production that leads to additional therapy61. Exacerbations also vary in severity, and can be categorized as mild, moderate, or severe according to the intensity of the medical intervention required to control the patient's symptoms. The indications of admission are listed in Table 2.
- Mild: controlled with an increased dosage of short acting bronchodilators only
- Moderate: controlled with short acting bronchodilators plus antibiotics and/or oral steroids
- Severe: patient requires hospitalization or visits the emergency room
2. Meaning and importance
Acute exacerbation of COPD can impact the natural course of COPD in the following ways:
- Worsening of quality of life
- Deterioration of symptoms and lung function (requiring a few weeks to recover)
- Acceleration of decline of lung function
- Increase in mortality rate
- Increase in socioeconomic burden
3. Etiology and risk factors
The causes of COPD acute exacerbation are numerous. The most common cause is respiratory infection (viral and/or bacterial)6263. Air pollution can also cause exacerbation. Discontinuing maintenance medication and poor adherence to COPD medication can also be causes. However, the cause of exacerbation cannot be identified in one-third of the cases. Diseases with similar symptoms (pneumonia, congestive heart failure, pneumothorax, pleural effusion, pulmonary thromboembolism, and arrhythmia) should also be differentiated from COPD exacerbations.
The COPD “Frequent exacerbator” phenotype is defined by two or more treated exacerbations per year, and the major predictor of frequent exacerbations is a history of prior exacerbations64. Other factors that have been associated with an increased risk of exacerbations include an increase in the ratio of the pulmonary artery to aorta cross sectional dimension65, a greater percentage of chest CT imaging-determined emphysema or airway wall thickness66 and the presence of chronic bronchitis6768.
4. Diagnosis and assessment of severity
Symptoms for COPD acute exacerbations are aggravation of dyspnea, increase in cough and sputum volume, and change in sputum color. Diagnosis of acute exacerbation is based on the presence of these symptoms that are beyond normal day-to-day variations, and a change in the patient's baseline medication regimens.
Severity of exacerbation can be assessed using the following variables.
1) History
- History of previous exacerbation frequency and severity
- Degree of air-flow obstruction in the stable state
- Duration and severity of deterioration of symptoms
- Comorbidity (especially, cardiac disease)
- Current medication
- Home O2 therapy
2) Physical examination
- Use of accessory muscle
- Paradoxical respiration, dyssynchrony between rib cage and abdomen
- Cyanosis
- Peripheral edema
- Hemodynamic instability
- Decrease of mentality
3) Laboratory findings
- Pulse oximetry: If oxygen saturation is below 90%, hospitalization should be considered. If respiratory failure is suspected, arterial blood gas analysis (ABGA) should be performed.
- Chest plain radiography: If there is a clear difference in the findings between the initial and follow-up radiographs, hospitalization should be considered.
- Electrocardiography should be performed to check for concomitant heart disease.
- Complete blood count: To check for anemia, polycythemia, and leukocytosis
- Blood chemistry: To check for electrolyte imbalance and hyperglycemia
- Sputum study: The characteristics of the sputum should be checked because antibiotic treatment may be necessary if the sputum is purulent. Culture tests may be helpful in selecting the antibiotics.
5. Medication
The goal for the treatment of COPD exacerbation is to alleviate the patient's symptoms of dyspnea, to stabilize respiratory status, to minimize the negative impact of current exacerbation, and to prevent future exacerbation.
Short-acting bronchodilators, systemic corticosteroids, and antibiotics are major three classes of medications for the pharmacologic treatment.
1) Bronchodilators
SABA with or without SAMA is recommended. Theophylline is not recommended.
2) Steroids
Systemic steroids can reduce the recovery and admission periods. They also improve lung function and oxygen saturation. Systemic steroids can also reduce further exacerbation. Although administration of 30–40 mg of prednisolone for 10–14 days is recommended, 5 days of oral steroids (40mg of prednisolone or equivalent) would be sufficient for treatment of COPD exacerbations6970. Intravenous administration is not superior to oral administration.
3) Antibiotics
Antibiotics are reported to reduce treatment failure and mortality. They are recommended when patients have three cardinal symptoms such as increase in dyspnea, sputum volume, and sputum purulence or two symptoms including increased purulence of sputum or for patients on mechanical ventilation71.
Initial choice of empirical antibiotic treatment is an aminopenicillin with clavulanic acid, or second or third generation cephalosporin, or advanced-generation macrolides.
In high risk patients (i.e., frequent exacerbators, severe lung function impairment, co-morbid cardiac disease, or admission to an intensive care unit), antibiotic choice includes a respiratory fluoroquinolone (levofloxacin, moxifloxacin, zabofloxacin). In a subgroup of patients who are at risk for infection by Pseudomonas aeruginosa, antipseudomonal antibiotics (ciprofloxacin, antipseudomonal cephalosporin, etc.) are needed.
The duration of the antibiotic treatment has not been well defined, but 5 to 7 days of treatment is as effective as long-duration treatment72.
6. Respiratory support
1) Oxygen
Oxygen therapy is a key component of management of COPD exacerbation. The target goal of saturation is 88%–92%. ABGA should be performed 30–60 minutes after oxygen therapy. However, too much oxygen can result in CO2 retention.
2) Ventilatory support
Some patients require admission to the intensive care unit (Table 3). Noninvasive positive pressure ventilation (NIPPV) or invasive mechanical ventilation (IMV) may be needed for such patients.
3) NIPPV
NIPPV is preferred over IMV. Success rate of NIPPV is reported to be 80%–85%. NIPPV improves respiratory acidosis, respiratory rate, and dyspnea. It also reduces complications, such as ventilator-associated pneumonia, and the duration of hospitalization. Moreover, NIPPV also reduces the IMV rate and mortality. The indications of NIPPV are listed in Table 4.
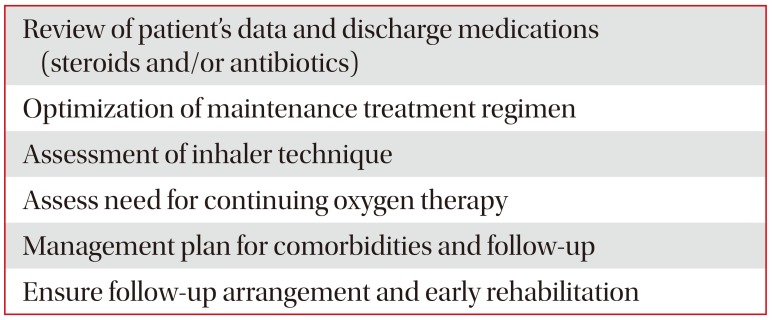
7. Hospital discharge and follow-up
Care bundles at hospital discharge are listed in Table 6. Education for smoking cessation, optimization of medication, assessment of the inhaler technique and need for continuing oxygen therapy, early rehabilitation post hospital discharge, and detailed follow-up plans are needed.
8. Prevention of exacerbations
COPD can be prevented by nonpharmaceutical and pharmaceutical treatments
1) Nonpharmaceutical treatment
- Pulmonary rehabilitation
- Smoking cessation
- Vaccination
- Lung volume reduction
2) Pharmaceutical treatment
- Inhaled long-acting bronchodilators: LABA or LAMA or LABA+LAMA
- ICS-containing regimens: ICS+LABA or ICS+LABA+LAMA
- PDE4 inhibitor
- Long term macrolides
- Mucoregulators: N-acetylcysteine, carbocysteine
Comorbidities of COPD
COPD patients are often accompanied by other diseases that may affect prognosis73747576. It is essential to identify and treat comorbidities in the management of COPD patients. The treatment of comorbidities in patients with COPD is not different from that in those without COPD.
Cardiovascular diseases are the most common and important comorbidities of COPD patinets7477. Ischemic heart disease, heart failure, arrhythmia, peripheral vascular disease, and hypertension are the most common. Beta-1 blockers are recommended as treatments to increase the survival rate of patients with heart failure. Patients with COPD should be prescribed a selective beta-1 blocker, which has proven safe for COPD patients78. Noninvasive positive ventilation improves the prognosis of patients with hypercapnic respiratory failure due to heart failure as well as COPD exacerbation79.
Even though osteoporosis is a major comorbidity in COPD77, it is often overlooked or its diagnosis is delayed80, worsening the general condition and prognosis. Since systemic corticosteroids significantly increase the risk of osteoporosis, frequent use of systemic corticosteroids should be avoided whenever possible.
Anxiety and depression are major comorbidities of COPD8182 and are associated with poor prognosis of COPD82. The prevalence of depression in Korean COPD patients is 17%–55%, which is higher than that of the general population (15.3%)838485. Korean Patient Health Questionnaire-9 is recommended as a screening tool to diagnose depression in patients with COPD868788.
The close link between COPD and lung cancer has been proven through several studies767789. The best way to prevent lung cancer in COPD patients is smoking cessation90. In the United States, lung cancer screening tests using low-dose chest CT in patients aged 55 to 74 years with a history of cigarette smoking of at least 30 pack-years, and, if former smokers, with a smoking cessation period of less than 15 years have improved survival rates9192. However, there have been concerns about overdiagnosis of benign nodules, mortality and morbidity resulting from biopsy of benign nodules, patient anxiety, and improper follow-up.
Metabolic syndrome and type 2 diabetes mellitus are very common in COPD patients. Diabetes mellitus has a negative effect on the prognosis of COPD patients75, leading to an increase in the length of hospital stay and mortality in exacerbation of COPD patients with diabetes93. Weight reduction aimed at achieving a body mass index of less than 21 kg/m2 is not recommended for patients with severe COPD.
Gastroesophageal reflux disease is often associated with COPD patients94, reducing the quality of life and increasing the risk of exacerbations649596. The prevalence of gastroesophageal reflux disease in Korean COPD patients is estimated to be 28%96.
Chest CT is widely used in patients with COPD, and the diagnosis of bronchiectasis is increasing97. Inhaled corticosteroids may have to be avoided in patients with bacterial colonization or recurrent lower respiratory tract infections.
Sleep deprivation is a common problem in COPD patients. Patients with COPD and obstructive sleep apnea syndrome (OSA) are referred to as COPD-OSA overlap syndrome. These patients have poorer quality of life and lower nighttime peripheral oxygen saturation than patients with isolated disease98, resulting in cardiac arrhythmia and pulmonary hypertension99100101. It has been reported that continuous positive airway pressure treatment for patients with COPD-OSA overlap syndrome reduces exacerbation and mortality of COPD102103.
As the elderly population grows, many people have two or more diseases at the same time, and COPD is a major disease of multiple diseases. It is important to simplify the medicines for those with multiple diseases.
Acknowledgments
We appreciate the effort of all the experts who participated in revising the COPD clinical practice guideline in 2018. The participants were the Korean Academy of Tuberculosis and Respiratory Diseases, Health Insurance Review and Assessment Service, Korean Physicians' Association, and Korea Respiration Trouble Association.
Notes
Authors' Contributions: Conceptualization: Oh YM, Yoo KH, Rhee CK. Methodology: Park YB, Yoon HK, Lim SY, Lee JH, Ahn JH. Formal analysis: Park YB, Rhee CK. Data curation: Rhee CK, Lee JH. Software: Rhee CK. Validation: Yoon HK, Ahn JH. Investigation: Park YB, Rhee CK, Yoon HK, Oh YM, Lim SY, Lee JH, Yoo KH, Ahn JH. Writing - original draft preparation: Rhee CK, Yoon HK, Oh YM. Writing - review and editing: Yoo KH, Oh YM. Approval of final manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.