Disseminated Mycobacterium intracellulare Infection in an Immunocompetent Host
Article information
Abstract
Disseminated Mycobacterium avium complex (MAC) infection can occur in immunocompromised patients, and rarely in immunocompetent subjects. Due to the extensive distribution of the disease, clinical presentation of disseminated MAC may mimic malignancies, and thorough examinations are required in order to make accurate diagnosis. We report a case of disseminated Mycobacterium intracellulare disease in an immunocompetent patient, which involved the lung, lymph nodes, spleen, and multiple bones. F-18 fluorodeoxyglucose positron-emission tomography imaging showed multiple hypermetabolic lesions, which are suggestive of typical hematogenous metastasis. However, there was no evidence of malignancy in serial biopsies, and M. intracellulare was repeatedly cultured from respiratory specimens and bones. Herein, we should know that disseminated infection can occur in the immunocompetent subjects, and it can mimic malignancies.
Introduction
Mycobacterium intracellulare is one of the Mycobacterium avium complex (MAC) and is the most frequently identified pathogen in nontuberculous mycobacterial (NTM) lung disease in the United States1. The infection is usually confined to the lung, but extrapulmonary or disseminated forms can occur, especially in immunocompromised patients but rarely in immunocompetent subjects2-4.
In case of disseminated MAC disease, in which clinical presentations could often mimic those of malignancies, the confirmative diagnosis should be made with a careful history taking and thorough examinations. Isolation of causative organisms is the first step to the correct diagnosis and F-18 fluorodeoxyglucose positron-emission tomography (FDG PET) can be useful to evaluate the extent of disease even though the main use of PET is to evaluate the extents of various malignancies5,6.
In this report, we describe a case of disseminated M. intracellulare infection in an immunocompetent male. The PET finding was so typical of hematogenous metastasis of malignancies, repeated histologic examinations were performed to exclude the possibility of malignancy.
Case Report
A 71-year-old man was referred to our hospital for the evaluation of recurrent fever, cough, sputum, shortness of breath, and recent weight loss of 3 kg (5% weight loss). Seven months ago, the patient was admitted to another hospital, and chest computed tomography (CT) revealed a 14-mm nodule and loculated effusion in left lower lung field. Under the diagnosis of empyema, drainage of pleural fluid concomitant with antibiotics therapy was performed and left pleural effusion and a lung nodule disappeared. However, the symptoms had recurred three months ago and persisted despite antibiotic treatment, and the patient was referred to our hospital for further evaluation. The patient had previously been healthy with no significant history of lung disease, other than a previously documented empyema and a lung nodule, and has smoked 20 cigarettes a day for 40 years. He was in mild respiratory distress, respiratory rate 24/min, temperature 37.6℃, and pulse 82/min. The lung sound was slightly diminished over left lower lung field.
Findings of laboratory studies showed a white-blood-cell count of 18,000/mm3 with 76.6% neutrophils, hemoglobin 10.8 g/dL, and platelet count 462,000/mm3. Electrolytes, measures of renal function, and liver enzymes were within normal limits. C-reactive protein (CRP) was elevated to 15.34 mg/dL. Serologic test for human immunodeficiency virus gave negative result. Initial blood and sputum cultures remained negative, but the patient was started on piperacillin/tazobactam (18 g per day) and ciprofloxacin (800 mg per day) as an empirical antibacterial therapy. Chest X-ray showed the ill-defined patchy mass opacity with surrounding ground-glass opacity in left mid-lung field (Figure 1). Chest CT showed huge mass-like consolidation in the lingular segment of left upper lobe and enlarged bilateral supraclavicular and mediastinal lymph nodes, suggestive of malignancy or inflammatory disease (Figure 2).
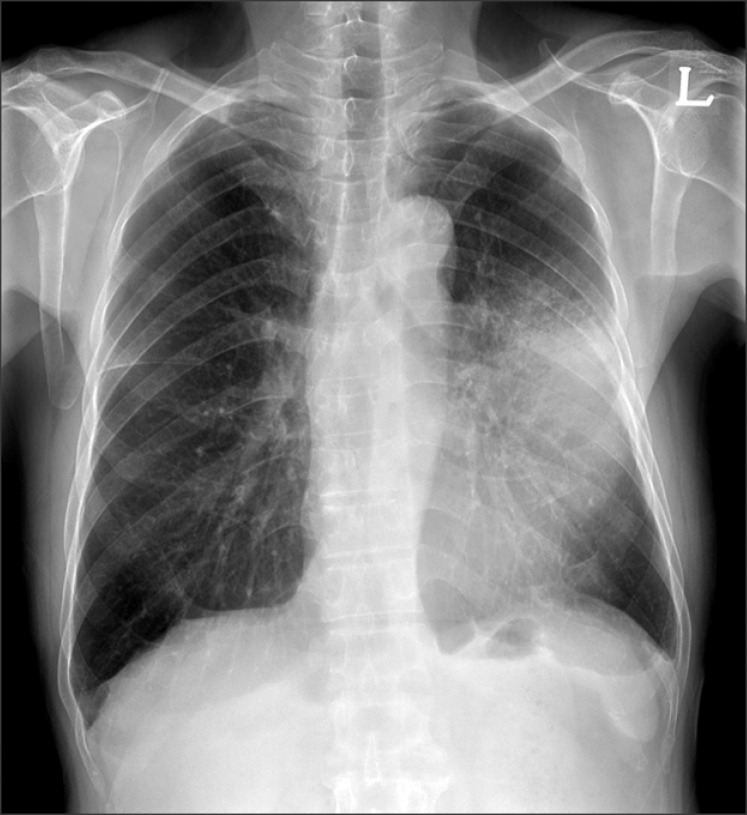
Chest X-ray showed the ill-defined patchy mass opacity with surrounding ground-glass opacity in left mid-lung field.

Contrast enhanced computed tomography showed consolidation in the lingual segment of left upper lobe (A) and bilateral meditational lymph nodes swelling (B).
During five days of antibiotic treatment, neither clinical nor radiologic improvement was observed. Brochoalveolar lavage (BAL) and endobronchial ultrasoundguided transbronchial needle aspiration (EBUS-TBNA) for paratracheal and subcarinal lymph nodes were performed, and the findings were unremarkable. The patient remained febrile after seven days of initial antibiotic therapy, and the regimen was changed to meropenem (3 g per day) and vancomycin (2 g per day). In addition to respiratory symptoms, the patient complained of back pain. Magnetic resonance imaging (MRI) of the thoracic and lumbar spine was performed and showed diffuse heterogenous low signal change with heterogenous enhancement (Figure 3). From this MRI finding, marrow infiltrative diseases such as multiple myeloma, malignant lymphoma, and multiple metastasis of unknown origin were considered. There was no evidence of monoclonal gammopathy based on serum and urine electrophoresis. FDG PET was performed and maximum intensity projection image showed multifocal hypermetabolic lesion in the lingular segment of left upper lung, bilateral supraclavicular and mediastinal lymph nodes, spleen, and multiple bones, including spine, right humerus, both scapula, left clavicle, sternum, sacrum, both pelvic bones, both femurs, and both side ribs (Figure 4). At this point, we had a high suspicion of hidden malignancy and performed percutaneous needle biopsy (PCNB) in the left upper lobe consolidation and left supraclavicular lymph node. However, both pathologies revealed nonspecific chronic inflammation and interstitial fibrosis and there was no evidence of malignancy or granulomas. Then, CT-guided bone biopsy was performed in the first lumbar vertebrae, and the pathology showed myeloid hyperplasia with marked plasmacytosis, without the evidence of malignant cell infiltration.
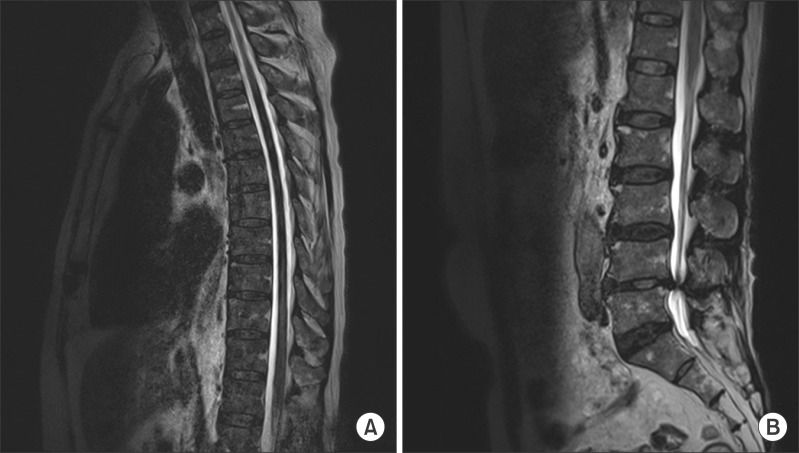
Magnetic resonance imaging of the thoracic (A) and lumbar (B) spine showed diffuse heterogenous low signal change with heterogenous enhancement.
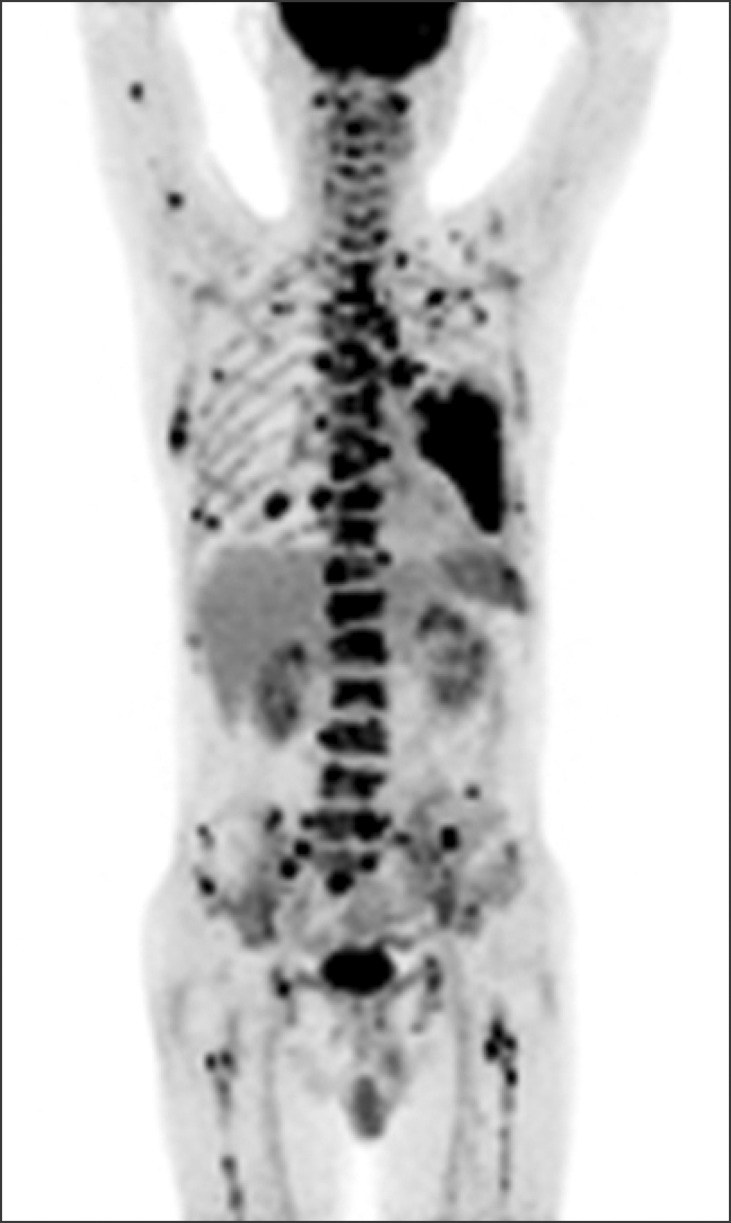
Maximum intensity projection image of F-18 fluorodeoxyglucose positron-emission tomography on admission showed multifocal hypermetabolic lesions in the left upper lung, lymph nodes, spleen, and multiple bones.
From the day of admission, serial sputum specimens were collected and cultured for mycobacteria using both mycobacteria growth indicator tuve (MGIT; Becton Dickinson Diagnostic Systems, Sparks, MD, USA) and Ogawa (Korean Institute of Tuberculosis, Seoul, Korea) media. On the day 30 of admission, acid-fast bacilli were repeatedly cultured in MGIT media and then in Ogawa media, which were identified as nontuberculous mycobacteria. Subsequent cultures from previous BAL and PCNB of left upper lobe consolidation specimens also were identified as nontuberculous mycobacterium. On the day 37 of admission, M. intracellulare was identified, and anti-MAC treatment was initiated with clarithromycin (1 g per day), rifampicin (600 mg per day), ethambutol (800 mg per day), and streptomycin (1 g per day). Even though the bone biopsy specimen did not reveal acid-fast bacilli, the reverse blot hybridization assay (REBA Myco-ID®; Molecules and Diagnostics, Wonju, Korea) using bone biopsy specimen revealed M. intracellulare. Later, M. intracellulare was also identified from bone biopsy specimen.
From these radiological and microbiological findings, the diagnosis of disseminated M. intracellulare infection was made. Anti-MAC therapy was continued and the patient was discharged with improved symptoms on the day 63 of admission. The drug sensitivity test revealed that the organism was susceptible to clarithromycin. The minimum inhibitory concentration of clarithromycin was 1 mg/L (susceptible). Unfortunately, additional information after discharge was not available due to transfer to another hospital.
Discussion
Disseminated MAC disease primarily occurs in immunocompromised patients, like those with acquired immunodeficiency syndrome, renal or cardiac transplantation, leukemia, or history of immunosuppressive therapy7. Recently, numerous disseminated MAC infection cases have been reported in immunocompetent hosts2,8,9.
The clinical symptoms of disseminated NTM infection include fever (>80%), night sweats (>35%), and weight loss (25%)10. The most commonly identified laboratory abnormalities include anemia and elevated levels of alkaline phosphatase, aspartate aminotransferase, lactate dehydrogenase, and CRP. In our case, mild anemia and CRP elevation were observed. The most commonly involved organs are the spleen, lymph nodes, liver, intestines, and bone marrow; the lungs are less commonly involved11. However, in a recent Taiwanese study by Chou et al.12, many patients (42.5%) with disseminated NTM infection had lung involvement and they explained that increased suspicion for pulmonary NTM infection and improved culture techniques may be the reason of increasing incidence. In our case, we also had positive cultures of M. intracellulare in sputum, BAL fluid, and lung parenchyma.
CT and MRI can well demonstrate multiple lesions of disseminated disease such as lymph nodes enlargement, splenomegaly, and bone marrow involvement. On the other hand, FDG PET can recognize whole body distribution more easily and importantly, can recognize lesions which show as normal in other imaging modalities. In our case of disseminated disease, CT finding of spleen was unremarkable, although FDG PET revealed a focal hypermetabolic lesion. FDG uptake increases when metabolic activity is increased by the presence of inflammatory cells, and there are several reports related to FDG accumulation in MAC infection13,14. Moreover, FDG PET can well demonstrate the activity of disseminated MAC, assess the treatment response after anti-MAC therapy, and provide suitable biopsy sites15.
The distribution of FDG accumulation is similar between disseminated MAC and other systemic diseases, such as malignancies and other granulomatous diseases. Therefore, histopathologic diagnosis is essential for further treatment. We performed four core needle biopsies in lung parenchyma, supraclavicular lymph node, and spines and EBUS-TBNA in enlarged mediastinal lymph nodes and there was no evidence of malignancy in any of these specimens.
In the initial period of evaluation, cultures in respiratory specimens were positive for NTM but bone biopsy specimen did not reveal NTM. Instead, molecular technique using REBA method detected M. intracellulare DNA from the bone biopsy specimen and later M. intracellulare was isolated from bone biopsy specimen. Hence, molecular technique may permit rapid diagnosis of disseminated NTM disease. In our case, REBA technique was used and rapid identification among NTM species was also possible by using this kit.
In conclusion, our report indicates that the clinical presentations of disseminated MAC infection can mimic those of malignancies. Thorough examinations, including histopathologic and microbiologic diagnosis, are required. FDG PET is a useful diagnostic tool to assess the exact extent of disease and provide suitable biopsy sites. Along with culture method, REBA is an improved rapid molecular diagnostic tool in identification of mycobacterium.