 |
 |
| Tuberc Respir Dis > Volume 72(4); 2012 > Article |
|
Abstract
Background
Chronic obstructive pulmonary disease (COPD) is now regarded as a heterogenous disease, with variable phenotypes. Acute exacerbation of COPD is a major event that alters the natural course of disease. The frequency of COPD exacerbation is variable among patients. We analyzed clinical features, according to the frequency of acute exacerbation in COPD.
Methods
Sixty patients, who visited Gyeongsang National University Hospital from March 2010 to October 2010, were enrolled. Patients were divided into two groups, according to their frequency of acute exacerbation. Frequent exacerbator is defined as the patient who has two or more exacerbation per one year. We reviewed patients' medical records and investigated modified Medical Research Council (MMRC) dyspnea scale, smoking history and frequency of acute exacerbation. We also conducted pulmonary function test and 6-minute walking test, calculated body mass index, degree of airway obstruction and dyspnea and exercise capacity (BODE) index and measured CD146 cells in the peripheral blood.
Results
The number of frequent exacerbators and infrequent exacerbators was 20 and 40, respectively. The frequent exacerbator group had more severe airway obstruction (forced expiratory volume in one second [FEV1], 45% vs. 65.3%, p=0.001; FEV1/forced vital capacity, 44.3% vs. 50.5%, p=0.046). MMRC dyspnea scale and BODE index were significantly higher in the frequent exacerbator group (1.8 vs. 1.1, p=0.016; 3.9 vs. 2.1, p=0.014, respectively). The fraction of CD146 cells significantly increased in the frequent exacerbator group (2.0 vs. 1.0, p<0.001).
Chronic obstructive pulmonary disease (COPD) is a slowly progressive disease characterized as not fully reversible airflow limitation1. COPD occurs by various pathogenesis, and also has various clinical features. Thus, it is classified into various phenotypes2. The stage of COPD is classified according to forced expiratory volume in one second (FEV1). However, as this classification has a limitation in the prediction of the severity or prognosis of the disease, various evaluation indices such as the quality of life and body mass index (BMI), degree of airway obstruction and dyspnea and exercise capacity (BODE) has been used3-5. The acute exacerbation of COPD is considered an index that reflects the severity of the disease. However, it is still controversial for whether acute exacerbation of COPD is an important phenotype6. Accordingly, this study was conducted to investigate who are more susceptible to acute exacerbation and its correlation with disease severity. In addition, CD146, a marker of circulating endothelial cells that has been known to increase in patients with COPD in previous studies, was measured to investigate its correlation with acute exacerbation of COPD7,8.
This study was conducted on COPD patients who visited the division of pulmonology of Gyeongsang National University Hospital from March 2010 to October 2010. Patients were diagnosed with COPD if FEV1/forced vital capacity (FVC) ratio was less than 70% after inhalation of short-acting bronchodilator according to the guideline on Global Initiative for Chronic Obstructive Lung Disease (GOLD). Subject inclusion criteria were as follows: current or ex-smokers with a smoking history of 10 pack years or higher, patients aged 40~80 years, and patients who were diagnosed with COPD and who had FEV1/FVC ratio<70%. Subject exclusion criteria were as follows: COPD patients with bronchial asthma, patients with structural pulmonary diseases such as severe bronchiectasis or tuberculous destroyed lung in chest X-ray, patients who were unable to complete a questionnaire themselves, patients who could not undergo 6-minute walk test, and patients with uncontrolled diseases that may affect study results. The subjects were divided into the frequent exacerbator group and infrequent exacerbator group, and then differences in clinical features were investigated between the two groups. Frequent exacerbator was defined as a patient with equal or more than two exacerbations per one year.
The subjects' age, gender, BMI, and smoking history were examined via the review of their medical records. As for the smoking history, the subjects were divided into the current smoker, ex-smoker, and never-smoker according to smoking status, and their total smoking amount was examined. The frequency of acute exacerbation for the recent one year was examined via the interview with the subjects. The Modified Medical Research Council (MMRC) scale was measured via a questionnaire. In this study, acute exacerbation was defined as an event requiring treatments with systemic steroid or antibiotics due to the rapid deterioration of respiratory symptoms such as cough, dyspnea, and sputum1. A pulmonary function test was conducted on all the subjects, and their disease stage was classified according to the GOLD guideline. 6-minute walk test was also conducted, and BODE index was measured. After achieving patients' informed consent, their blood samples were collected to measure CD146 level, a circulating endothelial cell marker. As for the measurement method, 10 mL of peripheral blood was collected from the subjects, and centrifuged to separate peripheral blood mononuclear cells. The peripheral blood mononuclear cells were then cultured with antibodies to CD146 for 30 minutes, followed by the quantitative analysis of CD146 using fluorescence activated cell sorting flow cytometry (Becton Dickinson and Company, Franklin Lakes, NJ, USA) and CellQuest software (Becton Dickinson and Company).
Each value was expressed as mean±standard deviation. An independent-samples t-test was conducted to compare pulmonary function, MMRC scale, 6-minute walk test, BMI, BODE index, and CD146 level between the frequent exacerbator group and infrequent exacerbator group. A chi-square test was conducted to compare gender, smoking history, and GOLD stage between the two groups.
The statistical analysis was conducted using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Differences were considered statistically significant if p<0.05.
A total of 60 COPD patients participated in the study. They consisted of 20 frequent exacerbators and 40 infrequent exacerbators. The subjects' mean age was 68.3±8.6 years and the male to female ratio was 57:3, which showed no significant difference between the two groups. The BMI was shown to be 21.3±2.4 and 22.6±3.9 in the two groups, respectively, which showed no significant difference. No significant difference in the previous and current smoking history was found between the two groups. In addition, no significant difference in the total amount of smoking was found between the two groups (45.3±38.9 pack years and 37.05±13.3 pack years, respectively) (Table 1).
The COPD stage that was determined according to the GOLD guideline was shown to be significantly higher in the frequent exacerbator group (p=0.015) (Table 1). The mean FEV1 of the frequent exacerbator group was shown to be 45.0±17.2% and that of infrequent exacerbator group was 65.3±21.8% (p=0.001). The FEV1/FVC ratio was shown to be 44.3±11.9% and 50.5±10.8% in the two groups, respectively, which was significantly lower in the frequent exacerbator group (p=0.046) (Figure 1).
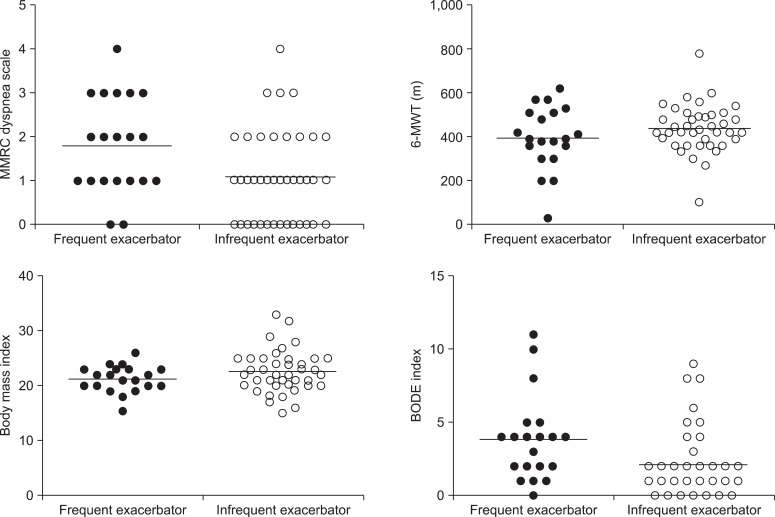
The MMRC scale was shown to be 1.8±1.1 and 1.1±1.0 in the two groups, respectively, which was significantly higher in the frequent exacerbator group (p=0.016) (Figure 2). 6-minute walk test and BMI showed no significant difference between the two groups (p=0.198 and p=0.162) (Figure 2). As a result of calculating the BODE index, it was shown to be 3.9±2.9 in the frequent exacerbator group, and 2.1±2.3 in the infrequent exacerbator group, which was significantly higher in the frequent exacerbator group (p=0.014) (Figure 2).
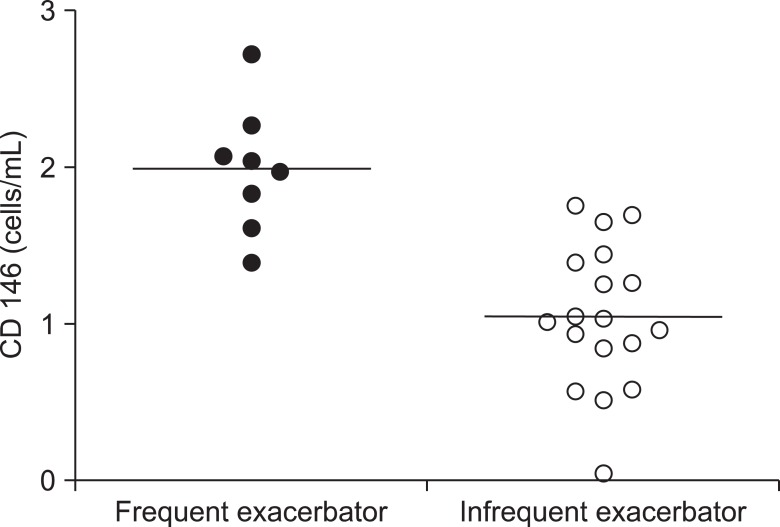
Twenty-six out of the 60 subjects agreed to blood collection, of whom eight subjects were frequent exacerbators and 18 subjects were infrequent exacerbators. The mean concentration of CD146 was shown to be 2.0±0.4 cells/mL in the frequent exacerbator group, and 1.0±0.5 cells/mL in the infrequent exacerbator group, which was significantly higher in the frequent exacerbator group (p<0.001) (Figure 3).
In this study, the COPD patients were divided into the frequent exacerbator group and infrequent exacerbator group, and then differences in the clinical features and CD146, a circulating endothelial cell marker, were compared between the two groups. Despite the unclear establishment of the definition of the acute exacerbation of COPD, the definition described in the GOLD guideline has been most commonly used. Thus, in this study, the definition was used according to the GOLD guideline1. In addition, the classification of frequent exacerbator group and infrequent exacerbator group has not been clearly established. Thus, in this study, the subjects were classified according to the mean frequency of acute exacerbation for the past one year. As shown in a study conducted by Hurst et al.9, the subjects were classified into the frequent exacerbator group if they had acute exacerbation twice or more during the past one year. The results of this study showed that the airway obstruction was more sever in the frequent exacerbator group than in the infrequent exacerbator group, and that the BODE index and CD146 concentration were higher in the frequent exacerbator group than in the infrequent exacerbator group.
Miravitlless et al.10 reported that the risk of acute exacerbation increased as airway obstruction became more severe. Cote et al.11 reported that airway obstruction was more severe in the patients with acute exacerbation than in the patients without acute exacerbation, and also reported that airway obstruction was more severe in the patients who had acute exacerbation twice or more than in the patients who had acute exacerbation once in a prospective study that was conducted on 205 COPD patients for 24 months. In this study, the disease stage according to the GOLD guideline was higher in the frequent exacerbator group than in the infrequent exacerbator group. In addition, the FEV1 and FEV1/FVC were lower in the frequent exacerbator group, which were consistent with the results of previous studies.
BODE index is comprised of FEV1, BMI, 6-minute walk test, and MMRC scale4. Cote et al.11 reported that BODE index was higher in patients with acute exacerbation than in patients without acute exacerbation. Hodgev et al.12 reported that the frequency of acute exacerbation had a significant correlation with BODE index, and that the BODE index was higher in the frequent exacerbator group than in the infrequent exacerbator group. In this study, the BODE index was higher in the frequent exacerbator group than in the infrequent exacerbator group, which indicates that acute exacerbation may more frequently occur in patients with high BODE index. No significant difference in the BMI and 6-minute walk test that are components of BODE index was found between the two groups in this study. Donaldson and Wedzicha13 and Cote et al.11 also reported that no significant difference in BMI and 6-minute walk test was found between the infrequent exacerbator group and frequent exacerbator group. On the other hand, Cote et al.11 reported that MMRC scale was higher in patients who had acute exacerbation twice or more than in patients who had acute exacerbation once for 24 months. In this study, the MMRC scale was also shown to be significantly higher in the frequent exacerbator group than in the infrequent exacerbator group.
Smoking is a major causative factor of COPD by deteriorating pulmonary functions. Vestbo et al.14 reported that smoking additionally caused annual reduction of pulmonary function of 21±4 mL in a study conducted on patients with moderate to severe COPD. Au et al.15 reported that smoking cessation reduced the frequency of acute exacerbation in COPD patients, and that risk reduction was correlated with period of smoking cessation in a study conducted on current and ex-smokers. However, no significant difference in the current and previous smoking history and smoking amount was found between the two groups in this study.
Circulating endothelial cell is an index that represents endothelial damage and dysfunction. It has been known to increase in patients with cardiovascular diseases such as acute myocardial infarction, pulmonary arterial hypertension, and stroke16-19. In addition, it has been reported to increase in patients with Behcet's disease, vasculitis such as systemic lupus erythematosus, infectious diseases such as sepsis, and various type of tumors20-23. Circulating endothelial cells have been known to increase in patients with COPD7,24. Sala et al.8 reported that circulating endothelial cells more increased in patients with acute exacerbation than in the control and patients with stable chronic pulmonary disease. Meanwhile, no study on the relationship between frequency of acute exacerbation and circulating endothelial cells has been conducted yet. In this study, the CD146 concentration was shown to have more increased in the frequent exacerbator group than in the infrequent exacerbator group, which showed that systemic vascular injury and dysfunction were more severe in the frequent exacerbator group.
In conclusion, compared to the infrequent exacerbator group, the frequent exacerbator group had more severe airway obstruction, higher BODE index, and higher CD146 level. Based on the aforementioned results, the acute exacerbation is likely to be one of the important phenotypes of COPD and a further study on CD146 is required.
References
1. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176:532-555. PMID: 17507545.


2. Friedlander AL, Lynch D, Dyar LA, Bowler RP. Phenotypes of chronic obstructive pulmonary disease. COPD 2007;4:355-384. PMID: 18027163.


3. Ståhl E, Lindberg A, Jansson SA, Rönmark E, Svensson K, Andersson F, et al. Health-related quality of life is related to COPD disease severity. Health Qual Life Outcomes 2005;3:56PMID: 16153294.



4. Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004;350:1005-1012. PMID: 14999112.


5. Ong KC, Earnest A, Lu SJ. A multidimensional grading system (BODE index) as predictor of hospitalization for COPD. Chest 2005;128:3810-3816. PMID: 16354849.


6. Soler-Cataluña JJ, Rodriguez-Roisin R. Frequent chronic obstructive pulmonary disease exacerbators: how much real, how much fictitious? COPD 2010;7:276-284. PMID: 20673037.


7. Huertas A, Palange P. Circulating endothelial progenitor cells and chronic pulmonary diseases. Eur Respir J 2011;37:426-431. PMID: 21282810.


8. Sala E, Villena C, Balaguer C, Ríos A, Fernández-Palomeque C, Cosío BG, et al. Abnormal levels of circulating endothelial progenitor cells during exacerbations of COPD. Lung 2010;188:331-338. PMID: 20082199.



9. Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010;363:1128-1138. PMID: 20843247.


10. Miravitlles M, Ferrer M, Pont A, Zalacain R, Alvarez-Sala JL, Masa F, et al. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax 2004;59:387-395. PMID: 15115864.



11. Cote CG, Dordelly LJ, Celli BR. Impact of COPD exacerbations on patient-centered outcomes. Chest 2007;131:696-704. PMID: 17356082.


12. Hodgev VA, Kostianev SS, Marinov BA. Correlation of frequency of exacerbations with the BODE index in COPD patients. Folia Med (Plovdiv) 2006;48:18-22. PMID: 17408072.

13. Donaldson GC, Wedzicha JA. COPD exacerbations. 1: Epidemiology. Thorax 2006;61:164-168. PMID: 16443707.



14. Vestbo J, Edwards LD, Scanlon PD, Yates JC, Agusti A, Bakke P, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med 2011;365:1184-1192. PMID: 21991892.


15. Au DH, Bryson CL, Chien JW, Sun H, Udris EM, Evans LE, et al. The effects of smoking cessation on the risk of chronic obstructive pulmonary disease exacerbations. J Gen Intern Med 2009;24:457-463. PMID: 19194768.




16. Erdbruegger U, Haubitz M, Woywodt A. Circulating endothelial cells: a novel marker of endothelial damage. Clin Chim Acta 2006;373:17-26. PMID: 16836991.


17. Mutin M, Canavy I, Blann A, Bory M, Sampol J, Dignat-George F. Direct evidence of endothelial injury in acute myocardial infarction and unstable angina by demonstration of circulating endothelial cells. Blood 1999;93:2951-2958. PMID: 10216090.



18. Bull TM, Golpon H, Hebbel RP, Solovey A, Cool CD, Tuder RM, et al. Circulating endothelial cells in pulmonary hypertension. Thromb Haemost 2003;90:698-703. PMID: 14515191.



19. Nadar SK, Lip GY, Lee KW, Blann AD. Circulating endothelial cells in acute ischaemic stroke. Thromb Haemost 2005;94:707-712. PMID: 16270621.


20. Camoin-Jau L, Kone-Paut I, Chabrol B, Sampol J, Dignat-George F. Circulating endothelial cells in Behcet's disease with cerebral thrombophlebitis. Thromb Haemost 2000;83:631-632. PMID: 10780331.



21. Clancy RM. Circulating endothelial cells and vascular injury in systemic lupus erythematosus. Curr Rheumatol Rep 2000;2:39-43. PMID: 11123038.



22. Mutunga M, Fulton B, Bullock R, Batchelor A, Gascoigne A, Gillespie JI, et al. Circulating endothelial cells in patients with septic shock. Am J Respir Crit Care Med 2001;163:195-200. PMID: 11208646.


23. Beerepoot LV, Mehra N, Vermaat JS, Zonnenberg BA, Gebbink MF, Voest EE. Increased levels of viable circulating endothelial cells are an indicator of progressive disease in cancer patients. Ann Oncol 2004;15:139-145. PMID: 14679134.



24. Peinado VI, Pizarro S, Barberà JA. Pulmonary vascular involvement in COPD. Chest 2008;134:808-814. PMID: 18842913.


Figure 1
Comparison of FEV1 (% predicted) and FEV1/FVC (%) between frequentand infrequent exacerbator (45.0±17.2 vs. 65.3±21.8, p=0.001 and 44.3±11.9 vs. 50.5±10.8, p=0.046). FEV1: forced expiratory volume in one second; FVC: forced vital capacity.
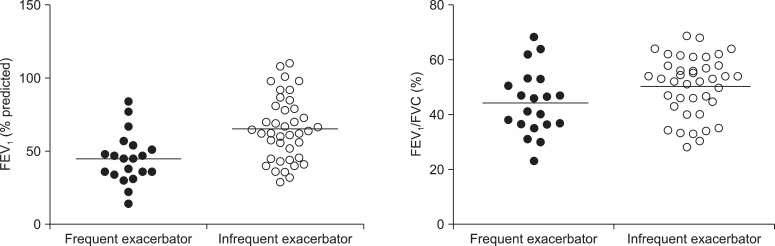
Figure 2
Comparison of MMRC dyspnea scale (1.8±1.1 vs. 1.1±1.0, p=0.016), 6-MWT (395.5±144.2 vs. 438.8±108.8, p=0.198), body mass index (21.3±2.4 vs. 22.6±3.9, p=0.162) and BODE index (3.9±2.9 vs. 2.1±2.3, p=0.014) between frequent and infrequent exacerbator. MMRC: modified Medical Research Council; 6-MWT: 6-minute walking test; BODE: body mass index, degree of airway obstruction and dyspnea and exercise capacity.
- TOOLS
-
METRICS

- Related articles
-
Clinical Studies on the Side Reaction of Pyrazinamide1968 September;15(3)


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



