 |
 |
| Tuberc Respir Dis > Volume 72(5); 2012 > Article |
|
Abstract
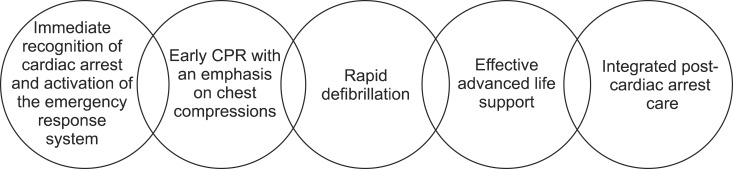
Cardiopulmonary resuscitation (CPR) is a series of life-saving actions that improve the chances of survival, following cardiac arrest. Successful resuscitation, following cardiac arrest, requires an integrated set of coordinated actions represented by the links in the Chain of Survival. The links include the following: immediate recognition of cardiac arrest and activation of the emergency response system, early CPR with an emphasis on chest compressions, rapid defibrillation, effective advanced life support, and integrated post-cardiac arrest care. The newest development in the CPR guideline is a change in the basic life support sequence of steps from "A-B-C" (Airway, Breathing, Chest compressions) to "C-A-B" (Chest compressions, Airway, Breathing) for adults. Also, "Hands-Only (compression only) CPR" is emphasized for the untrained lay rescuer. On the basis of the strength of the available evidence, there was unanimous support for continuous emphasis on high-quality CPR with compressions of adequate rate and depth, which allows for complete chest recoil, minimizing interruptions in chest compressions and avoiding excessive ventilation. High-quality CPR is the cornerstone of a system of care that can optimize outcomes beyond return of spontaneous circulation (ROSC). There is an increased emphasis on physiologic monitoring to optimize CPR quality, and to detect ROSC. A comprehensive, structured, integrated, multidisciplinary system of care should be implemented in a consistent manner for the treatment of post-cardiac arrest care patients. The return to a prior quality and functional state of health is the ultimate goal of a resuscitation system of care.
Cardiopulmonary resuscitation (CPR) refers to a series of emergency lifesaving actions which is performed in an effort to manually resuscitate a person in cardiac arrest. As CPR requires various emergency treatments in short time, the essential treatment procedures had been established as a standardized guideline. In 1962, the American Heart Association (AHA) had established "A Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care" for the first time and since then the efforts to medically improve CPR has been continued up to now, and it has been applied continually to CPR based on the research results known from many clinical studies. Thereafter, the International Liaison Committee on Resuscitation (ILCOR) which was constituted in 1993 had performed its tasks to apply new scientific grounds which were periodically accumulated at each 5 year from 2000 to the Guidelines for Cardiopulmonary Resuscitation and came to present an Integrated Guidelines, providing each country scientific grounds for revising or establishing their own CPR guidelines. Korea also had established and notified "A Common Guidelines for CPR" which was the first national guidelines for CPR in 2006. The AHA and ILCOR had developed a revised guideline for CPR in 20101-11 and based on it, Korea had developed a revised guideline for CPR in 201112. In this paper, key details concerning CPR for adult from the Guidelines for Cardiopulmonary Resuscitation of Korea 2011 were extracted and summarized.
Cardiac arrest in the form of sudden cardiac death is unpredictably incurring at places other than medical institutions. Because of the rapid ischemic damages to the body tissues including brain after cardiac arrest, it is necessary to perform a speedy resuscitation in order to restore the life. Therefore, all sectors should be engaged in integrated and intensive life saving actions which are including CPR by a witness, prompt response from the emergency medical services (EMS) systems, and professional treatment of medical institutions in order to increase the survival potential of patient with cardiac arrest while minimizing time delay.
The immediate prognosis after cardiac arrest can be classified into 3 stages depending on the time passage. The first stage is the time period of about 4 to 5 minutes from the incurrence of cardiac arrest. In this time frame, there is no tissue damage yet, if the heart rate is recovered, the patient can recover without any damage to bodily tissues. Therefore, if the prompt cardiac resuscitation including defibrillation for ventricular fibrillation (VF) is provided for the subject to regain return of spontaneous circulation (ROSC) in this time frame, it is highly likely to bring back heart beats and to restore spontaneous circulation as well. In addition to prompt CPR, the automatic external defibrillator (AED) should be used as soon as possible or contact EMS systems rapidly to make the defibrillator available on-site. The second stage is the time frame from 4~5 minutes to 10 minutes from the moment of cardiac arrest. In this time frame, the sudden energy exhaustion happens in tissues and ischemic tissue damage begins. Therefore, the most important step to treat in this time frame is CPR performance (especially, chest compression) to maintain oxygen supply to tissues. Also perfusion pressure to tissues should be maintained by performing specialized resuscitation including administering medication. The third stage is the time after 10 minutes had passed from cardiac arrest. In this stage, various metabolic factors are generated due to ischemic tissue damage, re-perfusion damages from performance of CPR. Various cytokines leaked into blood causes systemic reactions in similar form to systemic inflammatory response syndrome. Treatments of this stage are being attempted such as maintenance of perfusion pressure to tissues, administration of diversified medications to reduce damages to brain and tissues, but still there is no epoch-making treatment method available. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 indicates the need of efforts to reduce any additional brain damage by using therapeutic hypothermia after the patient is resuscitated.
Electrocardiogram (ECG) findings when any cardiac arrest had incurred, has association with the survival rate. Electric defibrillation at early stage has high survival rate for VF or pulseless ventricular tachycardia (ventricular arrhythmia). Whereas if there are ECG findings on asystole or pulse-less electrical activities, the survival rate will be lower than those found with VF or pulseless ventricular tachycardia. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 had reported that ventricular arrhythmia is found in about 25% of patients with cardiac arrest and in Korea the frequency of ventricular arrhythmia is ┬▒10%.
Bringing back the person with cardiac arrest to life requires a few key elements which should be connected with continuity and integration. The Chain of Survival refers to the connections of indispensable elements required for resuscitation of patient with cardiac arrest from the moments of its incurrence to coming back to life. If any of these elements composing the Chain of Survival is not performed properly, it is unlikely to revive the patient with cardiac arrest (Figure 1).
The first component in the Chain of Survival is the process from the incurrence of initial clinical symptoms in patient (loss of consciousness, abnormal or absent breathing with cardiac arrest, convulsive seizure) until arrival of emergency medical staff. This process involves that a bystander or a witness finding the patient immediately calls to EMS systems (119) about on incurrence of cardiac arrest, and the emergency medical dispatcher who got the report contacts available emergency service rescuer for dispatch to the site where the patient with cardiac arrest is located. Therefore, to ensure the first component of the Chain of Survival functions normally, it requires a call system to report on the emergency patient, and then a contact system for dispatch of emergency rescuer, fire-fighter or police as responding to the report made by calls. In addition, an ambulance should be available in readiness with equipments for emergency care and with space for the emergency rescuer to ride on at all times. Delayed identification on cardiac arrest will delay CPR performance and reporting to EMS systems, having bad effects on survival rate from cardiac arrest. Therefore, it requires to extend education on CPR which should be implemented with clinical profile details of cardiac arrest (in particular, agonal gasps, convulsive seizure can be the pattern of cardiac arrest) so as to ensure not to waste time in order to identify on cardiac arrest in actual situation. Emergency medical dispatcher should have been trained for capacity to explain and check the clinical profile of cardiac arrest in details upon reception of report for suspicion on the incident of cardiac arrest.
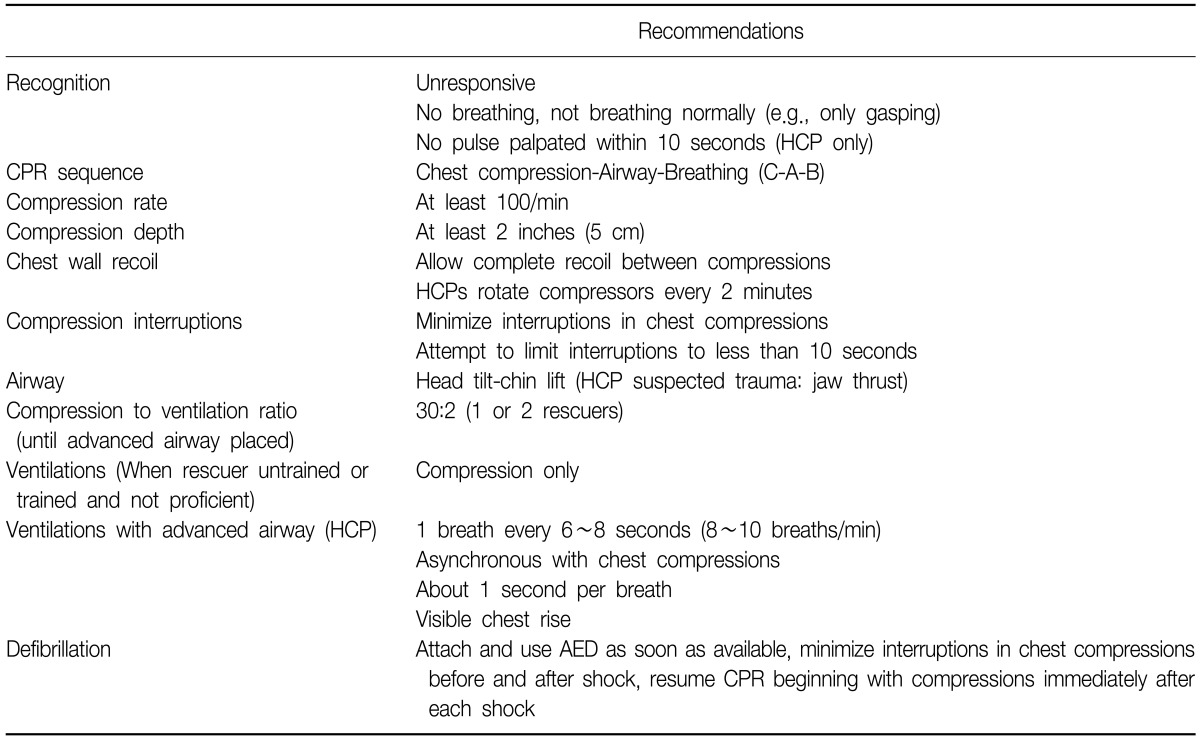
In rescuing a person having cardiac arrest, performing CPR promptly including chest compressions is an initiation step of resuscitating the patient with cardiac arrest. Anyone who witnesses person with cardiac arrest should begin the chest compressions. For the bystander who had not received any training on CPR, the emergency medical dispatcher guides the bystander for the process of chest compression. Recommended chest compression with sufficient depth is in a speed Ōēź100 times per minute ensuring to minimize any interruptions to the compression. During chest compression diastole, sufficient diastole should be allowed, but it should be careful not to have hyperventilation when using an artificial respiration. Chest compression only can have substantial effects of raising resuscitation rate, thereby, the importance that chest compression has should be emphasized to its full extent (Table 1).
Rapid use of defibrillator has quite important effects on prognosis of VF cardiac arrest. The Guidelines for Cardiopulmonary Resuscitation 2011 emphasizes that rapid use of defibrillator is an important Chain of Survival in treating cardiac arrest because the success rate of defibrillation decreases by 7 to 10% whenever defibrillation is delayed by 1 minute. Development and diffusion of the AED are dramatically improving survival rate from cardiac arrest caused by VF. AED is a device to defibrillate automatically by reading ECG of patient with attachment of paddle to patient, thereby anyone should be able to use it with just some training. Automated defibrillation is a technique to use medical equipment, but is classified into category for general public to perform it and being educated as an element of basic CPR. To perform defibrillation rapidly, it is recommended to place a defibrillator in ambulances of all forms, airport, school, large scale building and a stadium that can accommodate more than 10,000 people. Not only the emergency medical care workers but also the personnel working at public places where the AED is placed should be able to handle the AED.
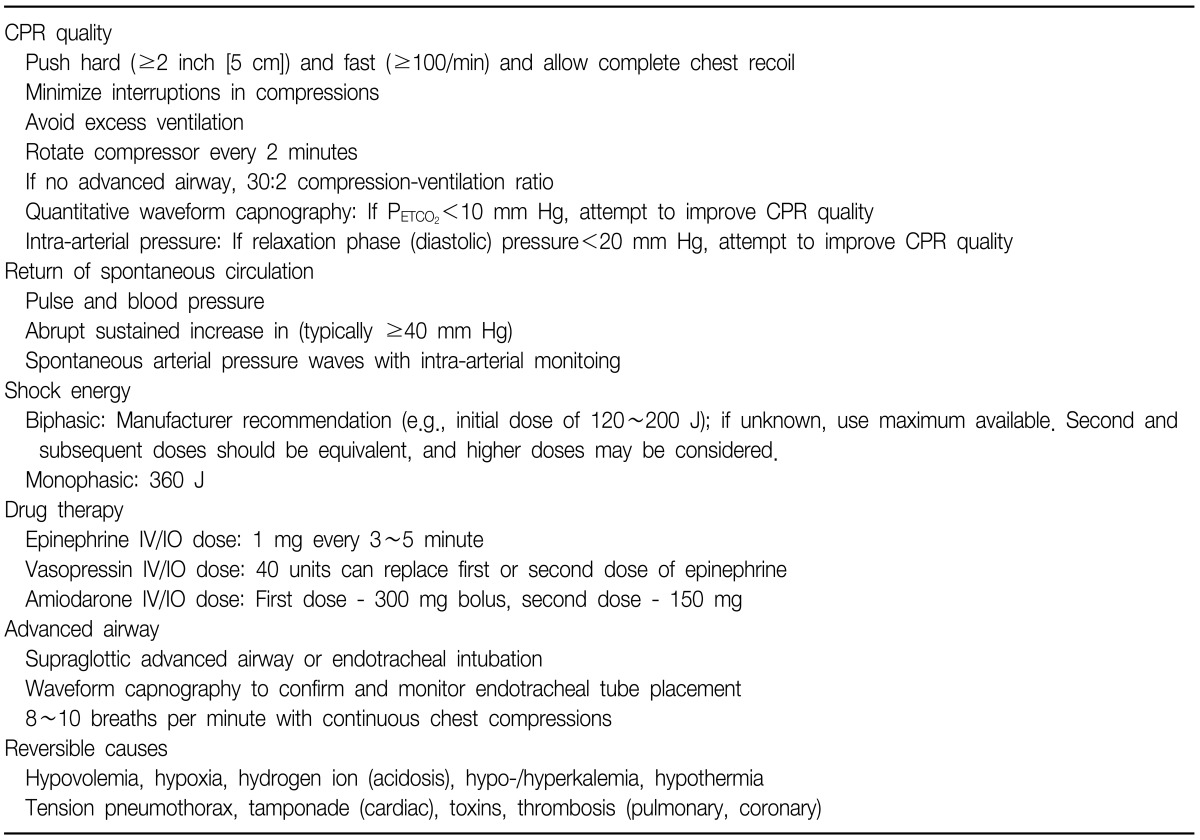
When CPR is in progress, various procedural techniques and drug administration should be performed quickly, therefore performing advanced CPR efficiently through team approach by multiple emergency medical care workers is important for resuscitation of patient in cardiac arrest. Advanced CPR should begin immediately if anyone can perform advanced CPR while basic CPR is in progress (Table 2).
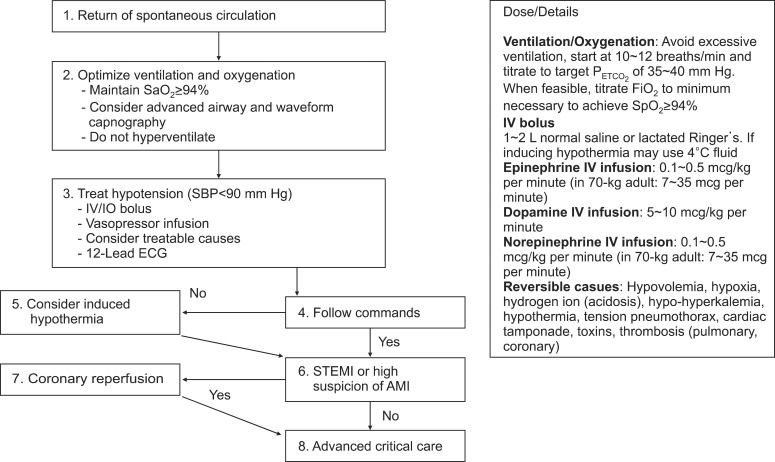
When CPR is attempted for patient in cardiac arrest, the patient may regain return of ROSC, however, the rate of discharged alive is low because in-hospital death rate is high due to the post-cardiac arrest syndrome even when a patient recovers from cardiac arrest. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 emphasizes the integrated post-cardiac arrest care is an important element of the Chain of Survival for raising the post-cardiac arrest survival rate which involves intensive care, therapeutic hypothermia, active intervention for coronary diseases and blood sugar level control after the subject regains ROSC, because such intensive and integrated treatment on the post-cardiac arrest syndrome reduces in-hospital death of patient with cardiac arrest and helps neurological recovery (Figure 2).
The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 is based on key contents of the Guidelines for Common CPR which was established in 2006. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 is a revised version of the Guidelines for Common CPR 2006 with amendments on the parts required modification due to emergence of new scientific evidences and the parts required adjustment for application in Korea among the contents of the Guidelines for Common CPR 2006. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 contains revisions that are oriented toward emphasis on the importance of chest compression, with simplified CPR procedures which can enable anyone to start CPR easily so as to raise survival rate from cardiac arrest. And the key details of revision includes change of basic CPR's sequence, introduction of chest compression only (Hands-Only) CPR, simplifying the cardiac arrest confirmation process and the basic CPR procedures, adjustment of chest compression methods and recommendation on active post-cardiac arrest treatment.
The Guidelines for Common CPR 2006 has recommended the order of basic CPR procedures as opening the airway (A)-checking on breathing and artificial respiration (breathing: B)-chest compression (C), i.e., in the order of A-B-C. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 has set the order of basic CPR procedures as Chest compression-Airway opening-artificial Breathing (C-A-B). The basic CPR in the order of A-B-C has been identified as delaying time to chest compression which is the most important step at early stage of cardiac arrest. Also, multiple by-standing rescuers tend to be reluctant to perform the mouthto-mouth artificial breathing, thereby some cases never perform the basic CPR in the order of A-B-C at all as it requires artificial breathing first in prior to the chest compression. So the basic CPR in the order of C-A-B is expected to reduce the possibility that by-standing rescuer will not perform CPR due to the burden of artificial respiration so that it will reduce the time consumption from incurrence of cardiac arrest to the chest compression.
Two elements of CPR, artificial respiration and chest compression only (hands-only or cardio-cerebral resuscitation) are indispensable life support methods for person in cardiac arrest. However, in the Guidelines for Cardiopulmonary Resuscitation of Korea 2011, it reports that performing the "Hands-Only CPR" (CPR in use of manual chest compressions only without artificial respiration) can increase survival rate of patient in cardiac arrest than the case with no CPR performed. It also reports when the Hands-Only CPR is performed to patient with cardiac etiology whose heart disease is presumed as the cause of cardiac arrest, the survival rate of such patient is similar to the survival rate of patient to whom the CPR together with artificial respiration is performed. Therefore, the "Hands-Only CPR" is recommended for the one who had been trained on CPR but is not confident to perform the entire procedures of artificial respiration and chest compression or the one who is reluctant to perform artificial respiration. However, it should be noted that artificial respiration should be performed together as essential for patient in cardiac arrest caused by respiratory arrest or drowning. When performing the chest compression only CPR, it is possible to simplify all processes of CPR into 3 stages of cardiac arrest confirmation-report-chest compression thereby it will increase acceptability of the general public for CPR.
Since CPR is required to begin rapidly in early stage after cardiac arrest is incurred, it is indispensable to reduce the time delay that happens in the process of confirming or recognizing on the incurrence of cardiac arrest as much as possible. In general, the person in cardiac arrest becomes unconscious immediately, non-responding to external stimulation, no breathing and no spontaneous movements. But immediately after the cardiac arrest, abnormal breathing (agonal gasps) can be observed temporarily or movement by convulsive seizure can be accompanied. Therefore, in the process of CPR training, the education should provide very detailed specifics of clinical profile in connection to cardiac arrest so as to prepare the trainees to be able to quickly recognize the incurrence of cardiac arrest when they witness it. In particular, the emergency medical dispatcher should be trained for ability to explain in details on the clinical profile of cardiac arrest to the one who is reporting, so that the dispatcher should be capable to figure out the situation being witnessed by the reporter on the event suspected as cardiac arrest. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 had simplified the basic CPR procedures. The Guidelines for Common CPR 2006 had recommended for rescuer to place his/her face close to the face of subject to "hear breathing sound, feel the breathe, and observe movement of chest (listen, feel and see)" in order to find out whether the person suspected with cardiac arrest is breathing or not. But in the Guidelines for Cardiopulmonary Resuscitation of Korea 2011, it is recommended to determine as cardiac arrest when any abnormal breathings (including agonal gasps) or no breathing is observed from the person suspected with cardiac arrest, and it had deleted the process of "listen, feel and see" to confirm on breathing.
The methods of chest compressions being recommended by the Guidelines for Cardiopulmonary Resuscitation of Korea 2011 do not have basically any differences from the methods provided by the Guidelines for Common CPR 2006. The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 recommends the chest compression depth as 5 cm (5 to 6 cm) at least in adults, and 5 cm in children in order to maintain the depth of chest compression and the compression ratio to appropriate level, and the ratio of chest compression is recommended to maintain at least 100 times per minute in both of adults and children.
The Guidelines for Cardiopulmonary Resuscitation of Korea 2011 recommends implementation of comprehensive and integrated treatment on the post-cardiac arrest syndrome incurring from most resuscitated patients. The post-cardiac arrest integrated treatment involves hemodynamic stabilization immediately after cardiac arrest, efficient treatment on the post-cardiac arrest syndrome incurred to each organs including brain (including therapeutic hypothermia), active intervention for acute coronary syndrome that is a major cause of cardiac arrest and prediction on neurological prognosis. Therapeutic hypothermia is applied to patient who is resuscitated from cardiac arrest and regained hemodynamic stability but still unconscious. It induces low body temperature in the range of 32~34Ōäā and maintains hypothermic state for 12 to 24 hours after incurrence of cardiac arrest. For the patient who is identified with ST-segment elevation myocardial infarction from ECG being recorded after resuscitation from cardiac arrest, coronary intervention should be performed immediately. When non ST-segment elevation myocardial infarction is incurred, coronary intervention should be considered. Immediately after being resuscitated, the mean arterial pressure should be maintained as Ōēź65 mm Hg, the arterial carbon dioxide tension should be maintained in the range of 40~45 mm Hg, and the arterial oxygen saturation should be maintained to 94~98% in order to minimize ischemia and re-perfusion damages. When conducting neurological examination to determine neurological prognosis, the fact that therapeutic hypothermia can have effects on the examination findings for prediction of neurological prognosis should be considered. For the post-cardiac arrest integrated treatment, if there is no additional risk in the process of transporting, it is recommendable to transfer the patient recovered from cardiac arrest to medical institutions where the facility for intensive post-cardiac arrest treatment is available.
References
1. Hazinski MF, Nolan JP, Billi JE, B├Čttiger BW, Bossaert L, de Caen AR, et al. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010;122(16 Suppl 2):S250-S275. PMID: 20956249.


2. Jacobs I, Sunde K, Deakin CD, Hazinski MF, Kerber RE, Koster RW, et al. Part 6: Defibrillation: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010;122(16 Suppl 2):S325-S337. PMID: 20956254.


3. Morrison LJ, Deakin CD, Morley PT, Callaway CW, Kerber RE, Kronick SL, et al. Part 8: Advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010;122(16 Suppl 2):S345-S421. PMID: 20956256.


4. Koster RW, Sayre MR, Botha M, Cave DM, Cudnik MT, Handley AJ, et al. Part 5: Adult basic life support: 2010 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2010;81(Suppl 1):e48-e70. PMID: 20956035.


5. Lim SH, Shuster M, Deakin CD, Kleinman ME, Koster RW, Morrison LJ, et al. Part 7: CPR techniques and devices: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2010;81(Suppl 1):e86-e92. PMID: 20956033.


6. Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S676-S684. PMID: 20956220.


7. Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S729-S767. PMID: 20956224.


8. Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S768-S786. PMID: 20956225.


9. Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, et al. Part 1: executive summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S640-S656. PMID: 20956217.


10. Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: adult basic life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S685-S705. PMID: 20956221.


11. Link MS, Atkins DL, Passman RS, Halperin HR, Samson RA, White RD, et al. Part 6: electrical therapies: automated external defibrillators, defibrillation, cardioversion, and pacing: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122(18 Suppl 3):S706-S719. PMID: 20956222.


12. The Korean Association of Cardiopulmonary Resusciation. The Korean Cardiopulmonary Resuscitation Guideline 2011. 2011. Seoul: Korean Association of Cardiopulmonary Resusciation.
- TOOLS
-
METRICS

- Related articles
-
Pulmonary Sequestration -Report of 1 Case-1988 June;35(2)
Principle of Pulmonary Function Tests1985 September;32(3)
Cardiopulmonary Exercise Testing: Basis of the physiology.2003 June;54(6)
Pulmonary Rehabilitation in COPD.2005 November;59(5)
A Case of Pulmonary Siderosis Mimicking Metastatic Lung Cancer.2011 January;70(1)


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



