Association between Participation in a Rehabilitation Program and 1-Year Survival in Patients Requiring Prolonged Mechanical Ventilation
Article information
Abstract
Background
The present study evaluated the association between participation in a rehabilitation program during a hospital stay and 1-year survival of patients requiring at least 21 days of mechanical ventilation (prolonged mechanical ventilation [PMV]) with various respiratory diseases as their main diagnoses that led to mechanical ventilation.
Methods
Retrospective data of 105 patients (71.4% male, mean age 70.1±11.3 years) who received PMV in the past 5 years were analyzed. Rehabilitation included physiotherapy, physical rehabilitation, and dysphagia treatment program that was individually provided by physiatrists.
Results
The main diagnosis leading to mechanical ventilation was pneumonia (n=101, 96.2%) and the 1-year survival rate was 33.3% (n=35). One-year survivors had lower Acute Physiology and Chronic Health Evaluation (APACHE) II score (20.2±5.8 vs. 24.2±7.5, p=0.006) and Sequential Organ Failure Assessment score (6.7±5.6 vs. 8.5±2.7, p=0.001) on the day of intubation than non-survivors. More survivors participated in a rehabilitation program during their hospital stays (88.6% vs. 57.1%, p=0.001). The rehabilitation program was an independent factor for 1-year survival based on the Cox proportional hazard model (hazard ratio, 3.513; 95% confidence interval, 1.785 to 6.930; p<0.001) in patients with APACHE II scores ≤23 (a cutoff value based on Youden’s index).
Conclusion
Our study showed that participation in a rehabilitation program during hospital stay was associated with an improvement of 1-year survival of PMV patients who had less severe illness on the day of intubation.
Introduction
As a result of improvements in life-saving medical resources in acutely critically ill patients, some patients receiving invasive mechanical ventilation (MV) become dependent on prolonged mechanical ventilation (PMV) [1] defined as the requirement for invasive MV for 21 days in intensive care unit (ICU) [2]. Patients requiring PMV display neuromuscular weakness, recurrent infections with multidrug-resistant bacteria, and delirium, consequently having a high long-term mortality rate [1,3,4].
PMV patients show ICU-acquired weakness. They require various medical resources for a long time during their hospital stays. Early and proactive rehabilitation of these patients is essential to reverse or minimize the impact of ICU-acquired weakness [5]. Technical developments of respiratory muscle rehabilitation in patients receiving long-term ventilator care have been reported [5-7]. They support the necessity of rehabilitation in the management of patients requiring long-term ventilator care.
Based on reported data [5-7], rehabilitation is associated with long-term outcomes of patients requiring PMV. However, there is a shortage of physiatrists, physiotherapists, nurses, and speech language therapists, and associated medical resources and facilities that are specialized in rehabilitation of patients requiring nonsurgical and long-term ventilator care in university hospitals in South Korea [8,9]. There are few studies on the effect of rehabilitation on outcomes of PMV patients. The present study hypothesized that participation in a rehabilitation program during a hospital stay could improve the long-term survival of PMV patients.
Thus, in this study, we evaluated the association between rehabilitation during a hospital stay (ICU and general ward) and 1-year survival in PMV patients whose main diagnoses leading to MV were various respiratory diseases in a regional center for respiratory diseases.
Materials and Methods
1. Study design and patient selection
This retrospective, observational study included patients admitted to a 12-bed adult respiratory ICU of a regional center for respiratory diseases of a university hospital that was established in December 2015. This center is located in a 1,200-bed university-affiliated tertiary care hospital. The respiratory ICU has full cardiovascular facilities and close airway monitoring equipment, with a nurse-to-bed ratio of 1:3. All subjects were managed according to therapeutic recommendations based on a lung-protective ventilator strategy [10]. All ventilated patients in the ICU were able to consult with physiatrists. They all had access to a rehabilitation program including full-time physiotherapy and physical rehabilitation provided by physiatrists. In addition, dysphagia treatment programs, including dietary texture modification, postural changes/compensatory maneuvers, and interventions designed to improve deglutition, were individually provided by physiatrists, physiotherapists, nurses, and speech language therapists.
Data from adult patients (aged ≥18 years) who were admitted to the respiratory ICU between December 1, 2015 and November 30, 2020 were retrospectively evaluated. To evaluate 1-year mortality rates after ICU admission, patient survival status was evaluated until March 10, 2022. Patients were finally included if they had received ventilator care for more than 21 days, regardless of their tracheostomy state [2]. Patients were excluded if they had irreversible brain injury or neuromuscular diseases, regardless of the length of ICU admission. The primary study outcome was 1-year survival rate after ICU admission.
2. Ethics approval
The study protocol was approved by the Institutional Review Board of Pusan National University Hospital (2208-004-117). The requirement for informed consent from enrolled patients or their families or surrogates was waived owing to the observational nature of this study. This study had no impact on the treatment of enrolled patients.
3. Data collection
Demographic and clinical data, including age, sex, body mass index, length of stay in the ICU and hospital, and in hospital mortality, were retrospectively obtained from electronic medical records (EMRs) of each subject. Illness severity was measured using Acute Physiology and Chronic Health Evaluation (APACHE) II score and accompanying organ failure was assessed using Sequential Organ Failure Assessment (SOFA) score [11,12], both of which were calculated based on laboratory and clinical data obtained within the first 24 hours of intubation.
Underlying comorbidities of all enrolled subjects at admission were obtained from their EMRs. In addition, Charlson’s weighted index was calculated to determine concurrent comorbidities prior to admission [13]. One-year cumulative mortality after ICU admission was assessed by reviewing the National Health Insurance Service database.
The number of patients who participated in a rehabilitation program directed by physiatrists and physiotherapists or speech language therapists was evaluated. In addition, the status of liberation of MV and independent ambulation and the recovery of deglutition functions at hospital discharge after the rehabilitation program were investigated.
Other factors evaluated from patients’ EMRs included main diagnosis leading to ventilator care, the status of tracheostomy, and total and out-of-pocket medical expenditures for all medical resources (including all medicines) during hospital (ICU and general ward) stay. Expenditures were reported in U.S. dollar (USD) based on the exchange rate on March 10, 2021 (1 USD equals 1,140.10 Korean won).
4. Statistical analysis
Normally distributed continuous variables are reported as mean±standard deviation. They were compared by Student’s t-test. Non-normally distributed continuous variables are reported as median (range). They were compared by the Wilcoxon rank-sum test. Categorical variables are reported as number (percentage). They were compared by chi-square or Fisher’s exact test, as appropriate. Patient survival was analyzed using the Kaplan-Meier method and compared using the log-rank test. Factors found to be significantly associated with 1-year survival were analyzed further with a Cox proportional hazard model to adjust for potential confounding effect of each factor. Hazard ratios with 95% confidence intervals were obtained. Optimal cutoff values for APACHE II and SOFA scores were determined based on the maximum Youden’s index [14]. All tests were two-tailed and p-values <0.05 were considered statistically significant. All statistical analyses were performed using IBM SPSS version 24.0 (IBM Corp., Armonk, NY, USA) and MedCalc Ver.20.109 (MedCalc Software, Ostend, Belgium) statistical software.
Results
1. Comparisons of clinical characteristics between PMV and non-PMV patients
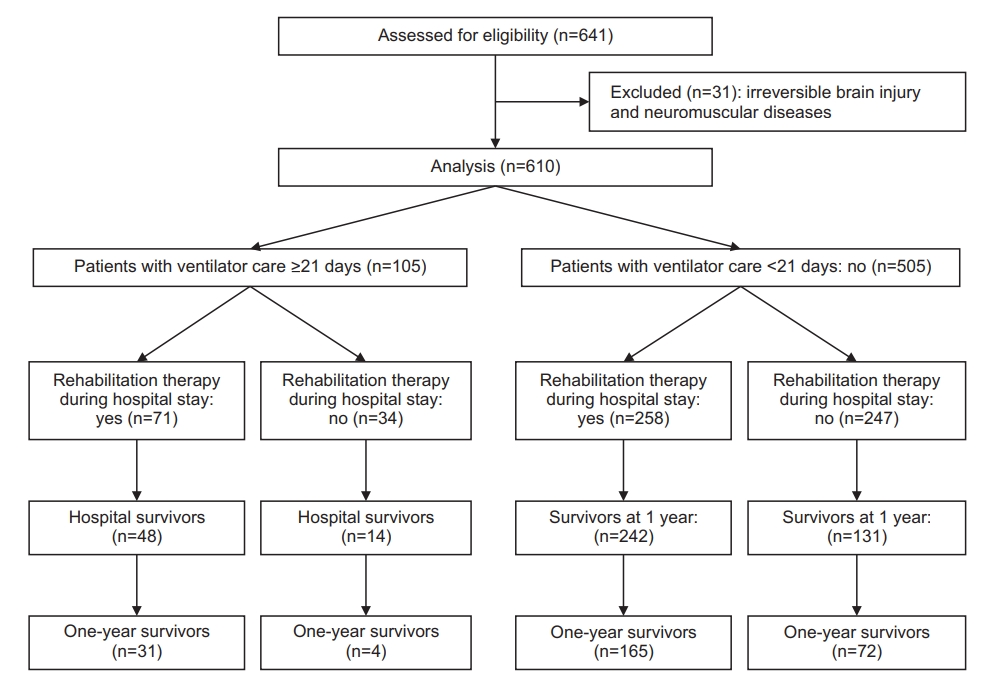
During the study period, 641 patients were deemed eligible for study participation. We excluded 31 patients with irreversible brain injury or neuromuscular diseases. Of 610 patients, 105 patients met our definition of PMV patients (Figure 1). Table 1 compares clinical characteristics of PMV and non-PMV patients. PMV patients had higher APACHE II scores and medical expenditures (total and out-of-pocket) than non-PMV patients. The percentage of patients who received tracheostomy and participated in a rehabilitation program during their hospital stay was higher in PMV patients than in non-PMV patients. However, higher percentages of PMV patients than non-PMV patients had ventilator-dependence and dysphagia at hospital discharge. In addition, the in hospital mortality and 1-year cumulative mortality rates of PMV patients were higher than those of non-PMV patients (Table 1).
2. Comparisons of survivors and non-survivors among PMV patients
We compared clinical characteristics of 1-year survivors and non-survivors (Table 2). Medical expenditures (total and out-of-pocket) did not significantly differ between the two groups. However, non-survivors had significantly higher APACHE II and SOFA scores on the day of intubation and higher rates of chronic lung diseases, cardiovascular diseases, and solid malignant tumors as comorbidities than survivors. Higher percentages of survivors than non-survivors underwent a rehabilitation program. In addition, higher percentages of survivors than non-survivors were liberated from a mechanical ventilator. Moreover, higher percentages of survivors than non-survivors did not have a swallowing problem at hospital discharge.
3. Participation in a rehabilitation program in PMV patients
In analysis of PMV patients, 71 patients underwent a rehabilitation program. The median duration of this program was 19 days (range, 1 to 150). When these patients were divided into those with and without rehabilitation program during hospital stay, patients who received this rehabilitation program had significantly longer hospital length of stay, higher rate of diabetes as comorbidity, higher total medical expenditure, and higher rate of liberation from ventilator than those who did not receive such rehabilitation program (Table 3).
4. Association between participation in a rehabilitation program and 1-year survival in PMV patients
Table 4 shows factors independently predictive of 1-year survival in PMV patients according to a Cox regression hazard model. Participation in a rehabilitation program during hospital stay was associated with 1-year survival in total patients based on multivariate Cox regression analysis. The Kaplan-Meier estimate of survival at 1 year was also consistent with a survival benefit of the rehabilitation program (Figure 2).

Univariate and multivariate analyses of factors associated with 1-year survival in patients requiring prolonged mechanical ventilation
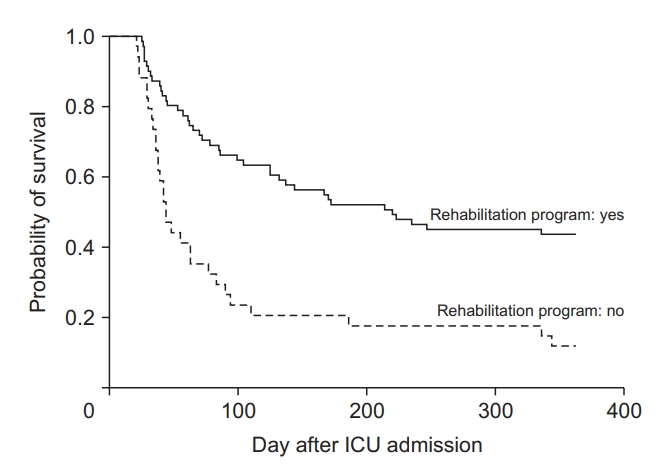
Kaplan-Meier curves of 1-year survival after the day of intubation according to whether patients participated in a rehabilitation program during hospital stay (log-rank, 18.133; p<0.001).
Survivors had significantly lower APACHE II scores at ICU admission. Therefore, subgroup analyses were performed for patients with less severe illness. In patients with APACHE II scores ≤23 (the cutoff value was based on the maximum Youden’s index [sensitivity 77.1%, specificity 50.0%, p=0.003]), participation in the rehabilitation program during hospital stay was associated with 1-year survival. However, in patients with APACHE II scores >24, there was no association between participation in the rehabilitation program and 1-year survival (Table 4).
Discussion
The present study evaluated the effect of participation in a rehabilitation program during hospital stay on 1-year survival in PMV patients. Our findings showed an association between participation in the rehabilitation program during hospital stay and improved 1-year survival. In subgroup analyses, participation in the rehabilitation program during hospital stay was associated with improved survival of PMV patients with lower APACHE II scores on the day of intubation and no cardiopulmonary comorbidities before hospital admission. Although PMV patients had a higher 1-year mortality rate and medical expenditures than non-PMV patients, participation in a rehabilitation program during hospital stay was associated with an improvement of long-term survival of PMV patients who had no cardiopulmonary comorbidities with less severe illness at ICU admission.
Use of medical resources, reflected by medical expenses, and long-term mortality were higher in PMV patients than in non-PMV patients. In Korean ICUs, there are few specialized physiatrists, physiotherapists, nurses, and speech language therapists for non-traumatic and nonsurgical patients requiring prolonged ventilator care. The present study tried to find other subgroups of patients (such as those with or without organ failure and those with or without underlying comorbidities) for whom a rehabilitation program benefited the 1-year survival. However, it was difficult to determine the effect of a rehabilitation program on 1-year survival because the number of patients was small. Therefore, it is necessary to determine subgroup(s) of patients who participated in a rehabilitation program during hospital stay and showed improved long-term outcomes by conducting a multicenter study.
Some prognostic models for predicting 1-year mortality of PMV patients have been developed using their clinical variables. The ProVent score based on four variables readily assessed on day 21 of MV (namely, a requirement for dialysis, a requirement for vasopressors, age ≥50 or ≥65 years, and a platelet count <150×109/L) for predicting 1-year mortality has been validated [3,4,15]. The extended ProVent model, which includes comorbidities and laboratory data (albumin and bilirubin), has been developed [16]. In addition to these clinical variables on day 21 of MV and underlying comorbidities, our data suggest that participation in a rehabilitation program during hospital stay is a valuable prognostic factor. Therefore, new predictive models for PMV patients using clinical variables, underlying comorbidities, and rehabilitation program status need to be developed based on large-scale multicenter studies.
ICU rehabilitation has recently emerged as an important field in critical care [17]. Protocolized rehabilitation directed toward an early mobilization and ventilator liberation protocol is recommended as an international guideline [18]. Although ICU rehabilitation could improve survival of patients with sepsis in Korea [19], there is no nationalized guideline regarding a rehabilitation program during ICU stays. Moreover, rehabilitation-related medical expenses have not been implemented by the Korean government. To avoid delayed initiation of rehabilitation programs and to improve long-term outcomes in chronically critically ill patients (including PMV patients), rehabilitation-related medical expenses for critically ill patients should be formally implemented.
The present study has several limitations. First, its retrospective design might have resulted in a selection bias. Second, this study included patients hospitalized in a single ICU. In addition, our results might not be generalizable to other settings such as patients requiring PMV after surgery or trauma. Therefore, additional studies of larger numbers of patients are needed to validate the effect of a rehabilitation program on long-term survival. Third, we hypothesized that early tracheostomized PMV patients would benefit more from a rehabilitation program than late tracheostomized patients because early tracheostomy in patients requiring long-term ventilator care is associated with improved patient comfort and reduced sedative drug use [20-22]. However, we could not find any associations between early tracheostomy and long-term survival due to a small number of enrolled patients.
In conclusion, this study evaluated the association between participation in a rehabilitation program during the hospital stay and 1-year survival in PMV patients. Our study suggests that a rehabilitation program could elicit a more beneficial effect on 1-year survival in PMV patients with less severe illness on the day of intubation who have no cardiopulmonary comorbidities. Large-scale multicenter studies are needed to evaluate the effect of a rehabilitation program on long-term outcomes of PMV patients requiring ventilator care for various reasons.
Notes
Authors’ Contributions
Conceptualization: Yoo W, Lee K. Methodology: Yoo W, Jang MH, Kim SH, Lee K. Formal analysis: Yoo W, Jo EJ, Mok J, Kim MH. Data curation: Yoo W, Kim S, Eom JS. Software: Yoo W, Jo EJ, Eom JS, Mok J, Kim MH. Validation: Yoo W, Jang MH, Kim SH. Investigation: Jo EJ, Eom JS, Mok J, Kim MH. Writing - original draft preparation: Yoo W, Jang MH, Kim SH. Writing - review and editing: Yoo W, Lee K. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
This work was supported by Pusan National University Research Grant, 2022.