Prevalence and Impact of Comorbidities in Individuals with Chronic Obstructive Pulmonary Disease: A Systematic Review
Article information
Abstract
This study aimed to describe the prevalence of comorbidities associated with chronic obstructive pulmonary disease (COPD) and their relation with relevant outcomes. A systematic review based on the PRISMA methodology was performed from January 2020 until July 2021. The MEDLINE, Lilacs, and Scielo databases were searched to identify studies related to COPD and its comorbidities. Observational studies on the prevalence of comorbidities in COPD patients and costs with health estimates, reduced quality of life, and mortality were included. Studies that were restricted to one or more COPD pain assessments and only specific comorbidities such as osteoporosis, bronchitis, and asthma were excluded. The initial search identified 1,409 studies and after applying the inclusion and exclusion criteria, 20 studies were finally selected for analysis (comprising data from 447,459 COPD subjects). The most frequent COPD comorbidities were: hypertension (range, 17%–64.7%), coronary artery disease (19.9%–47.8%), diabetes (10.2%–45%), osteoarthritis (18%–43.8%), psychiatric conditions (12.1%–33%), and asthma (14.7%–32.5%). Several comorbidities had an impact on the frequency and severity of COPD exacerbations, quality of life, and mortality risk, in particular malignancies, coronary artery disease, chronic heart failure, and cardiac arrhythmias. Comorbidities, especially cardiovascular diseases and diabetes, are frequent in COPD patients, and some of them are associated with higher mortality.
Introduction
Chronic obstructive pulmonary disease (COPD), a chronic respiratory disease is one of the most prevalent chronic diseases and is the fourth leading cause of mortality worldwide [1]. COPD patients often have comorbidities. which are associated with worse outcomes such as impaired quality of life, increased frequency of hospital admissions, worse therapeutic response, and even increased mortality [2-4].
However, the pathophysiological processes involved in the relationship between COPD and its comorbidities. Probable causes of the high prevalence of comorbidities in COPD patients are hypothesized and generally categorized by: advanced age, physical inactivity, poor diet, smoking, hypoxia, and systemic inflammation [5-10].
Studies describing comorbidities in COPD reported significant variability in not only the prevalence of different comorbidities but also the intensity of association between them [11]. In general, the presence of comorbidities is associated with the worst prognosis, but the impact of different comorbidities on outcomes varies significantly. Identification of the type of comorbidity and the possible clinical impact on the risk of exacerbations, impairment in quality of life, reduction of physical activity, and increased mortality, might help clinicians to improve the care of COPD patients.
This systematic review aimed to describe the estimated prevalence of comorbidities in COPD and their association with the relevant outcomes such as the use of health resources, quality of life, symptoms, exercise capacity, exacerbations, and mortality. To accomplish this, exploratory and quantity methodologies were applied.
Materials and Methods
This systematic review was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) [12] protocol. The studies were searched in the electronic databases MEDLINE-PubMed (Medical Literature Analysis and Retrieval System Online), Lilacs (Latin Literature and the Caribbean of Ciencias de la Salud), and Scielo (Scientific Electronic Library Online) - by the Virtual Health Library Brazil. To construct this research, the Patient, Intervention, Comparison, and Outcome (PICOS) strategy was required as an acronym for Population (individuals with COPD) and Intervention - or Exposure, for observational studies (comorbidities), Comparison (individuals without COPD), “Outcomes” - outcomes (exacerbations, hospitalizations, health costs, reduced quality of life and mortality), and “Study design” - study design (observational studies) [13]. The following keywords were used: pulmonary disease, chronic obstructive; comorbidity; observational studies as a topic, synonyms, and related words added by the Boolean operators “AND” and “OR” (Supplementary Table S1). No search strategies from the previous reviews were used. The period full search for the articles was carried out from January 2020 to July 2021, using the words found in the titles and article’s abstracts.
The relevant articles, collected through database searches, were selected by their main titles (first stage), abstracts (second stage), and complete and full reading of the selected material (third stage). An exploratory reading of all the selected materials was made, and, later, a selection and more analytical reading of the parts that were the most relevant for the review. Observational studies that estimated the prevalence of comorbidities in individuals with COPD and associated with exacerbations, hospitalizations, healthcare costs, reduced quality of life, and mortality were included. Articles that used primary or secondary data, published between 2003 and 2020, and that were available in English, Portuguese, or Spanish were also included in the data collection and added to the reading references for this study.
Studies that were restricted to evaluating individuals with COPD and only one more specific comorbidity such as osteoporosis, bronchiectasis, asthma, or pain were excluded. The other exclusion criteria followed the PRISMA methodology: duplicate studies which were removed and also the ones that described the same or very similar results from the same database. In addition, studies that did not list the comorbidities or their frequencies and studies that evaluated patients with respiratory diseases other than COPD [12] were excluded. Mendeley - Reference Management Software was used to deduplicate records from several database searches.
All the results related to outcomes were presented, even if they came from the same database, and this circumstance was indicated in the results. We opted to select all the results related to the outcomes, including those from the same database. Nevertheless, their circumstances are quoted in the results of the present study.
The process of identifying the methodological aspects and extracting data from the articles was accomplished by two independent reviewers (N.C.S. and F.W.R.C.). When there was any disagreement between them, the reviewers read the entire article again for reassessment. When there was a disagreement, a third independent reviewer evaluated the article and made the final decision.
After the article was completed, the search was last updated in December 2021, using the publication date filter present in the databases. This way, it was possible to evaluate the articles published after the analysis of the previous articles.
The quality of the included studies was elaborated using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [14]. The protocol for the construction stages of this systematic review was published in the International Prospective Register of Systematic Reviews (PROSPERO), under registration no. CRD42018081641.
Results
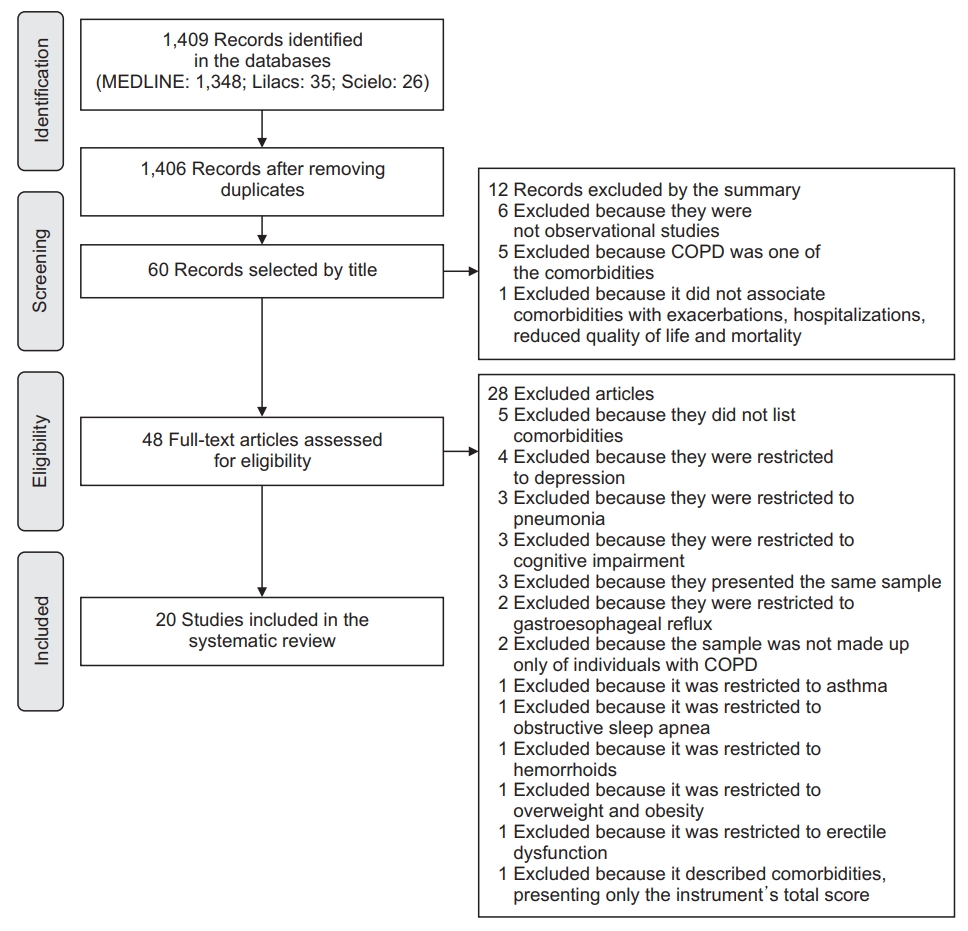
The initial search resulted in 1,409 articles (MEDLINE, 1,348; Lilacs, 35; Scielo, 26), and later 1,406 records after removing the duplicated ones. In these studies, 60 articles were selected by title screening. Twelve of the 60 were excluded because the abstract did not fit the selection criteria, leaving 48 articles for a full reading. Of the 48, 28 of them did not meet all the inclusion criteria, resulting in the final selection of 20 articles as shown in Figure 1.
1. Characteristics of the studies
The characteristics of the 20 articles selected are presented in Table 1. Of the 20 articles, most of them were cohort studies, with 11 retrospective and three prospective, four cross-sectional observational and two case- control [11,15-33]. Data from 637,827 subjects were included. Only one study did not show the number of participants, with the number of admissions as a sample (47,404,700) [15].
2. Used instruments
In the 20 articles, the researchers evaluated medical records while the others used different instruments. In one of these articles, a list of the comorbidities of interest was produced [19], while seven others used the COPD specific comorbidity test (COTE Index) [16], Charlson Comorbidity Index [19,21,24,27,32]. Five of these studies [11,18,22,23,27] used other instruments that were not designed to assess comorbidities such as the Modified Medical Research Council, mMRC [18,23] (dyspnea assessment); the St George’s Respiratory Questionnaire for COPD patients, SGRQ-C [18,23] (quality of life); Health-related quality of life - HRQoL-15D [22] (quality of life); Airways questionnaire 20, AQ20 [22] (quality of life); Hospital Anxiety and Depression Scale, HADS [27] (emotional state); Body mass index, Airway Obstruction, Dyspnea, and Exercise capacity, BODE [16,18,23] (health status and risk of death); and 6-minute walk test, 6MWT [11,18,23] (functional capacity).
3. Methodological quality
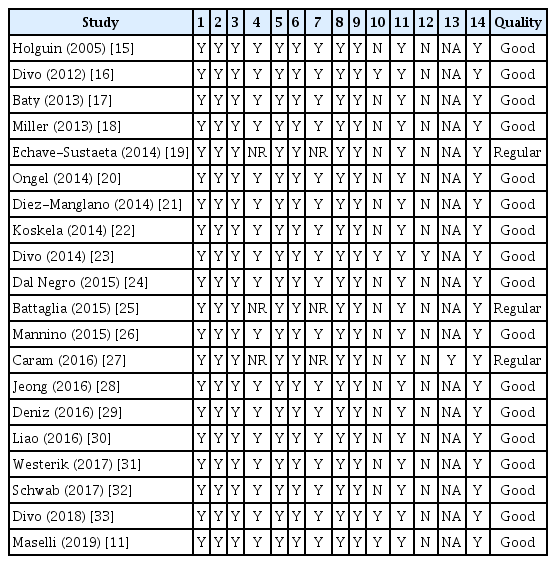
All the selected articles presented the research question or objective clearly, the population was well defined and the participation rate of the eligible people was at least 50%. In all the studies, the measures of exposure and results were clearly defined, valid, reliable, and implemented consistently. The main variables were measured and adjusted statistically for their impact on the relationship between exposure and outcome in all the studies, as shown in Table 2.
Only three articles did not report the period of selection and recruitment of the participants [19,25,27], and it was also not possible to understand whether the period was long enough to reasonably expect an association between exposure and outcome. Four articles evaluated exposure more than once through time [11,16,23,33]. In one of the studies, the evaluators of the results were blinded to the exposure status of the participants [23] and only one showed loss to follow-up [27]. Seventeen studies were classified as good methodological quality and three as regular (Table 2).
4. Comorbidities and outcomes
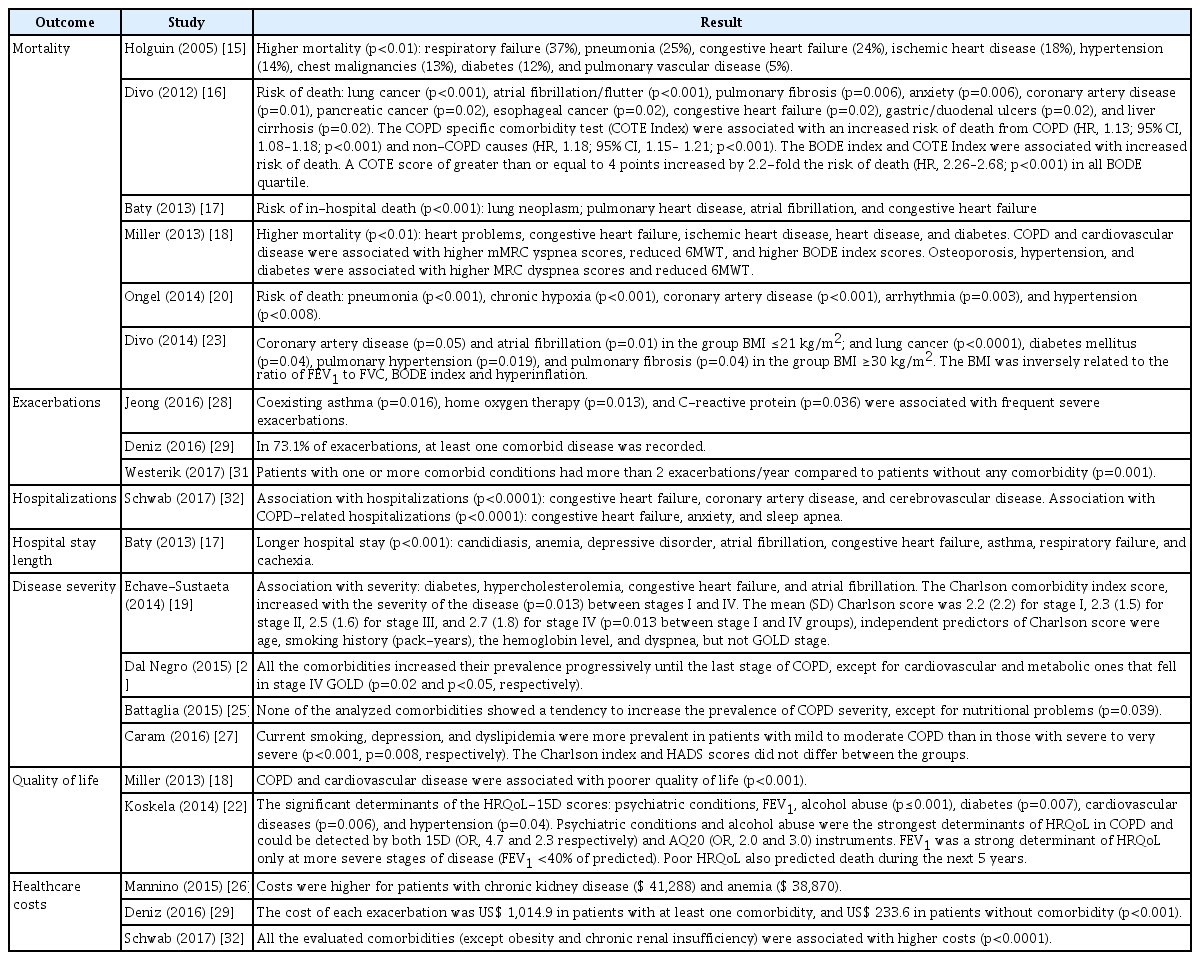
The prevalence of comorbidities in COPD patients are shown in Table 3. The most prevalent were hypertension (17%–64.7%), coronary artery disease (19.9%– 47.8%), and diabetes mellitus (10.2%–45%).
Six studies [15-18,20,23] showed increased mortality based on the presence of comorbidities, in particular malignancies, coronary artery disease, and cardiac arrhythmia. Four studies [28,29,31,32] indicated a role of comorbidities in the frequency and severity of exacerbations and one of them demonstrated a longer length of hospital stay for an exacerbation in patients with comorbidities [17]. Four studies showed an increased severity of COPD associated with more frequent comorbidities [19,24,25,27]. In general, the Charlson comorbidity index was higher in patients with more severe COPD. Two studies suggested an impact of comorbidities on quality of life [18,22], specifically, cardiovascular and psychiatric comorbidities. Lastly, three studies [26,29,32] indicated that healthcare costs were higher in patients with comorbidities. The impact of comorbidities on outcomes of COPD is summarized in Table 4.
Discussion
Our systematic review results showed that COPD patients are frequently affected by comorbidities and the most common are: cardiovascular diseases [11,15-17,22-26,28-33] (mainly hypertension, coronary artery disease, chronic heart failure, peripheral arterial disease, arrhythmia, and atrial fibrillation), metabolic diseases [15,17-19,21-28,32,33] (diabetes, hyperlipidemia, chronic kidney disease, and obesity), osteoarticular [11,18,23,24,26,28-33] (osteoarthritis and osteoporosis), respiratory [11,15,16,24,26,28,29,32] (obstructive sleep apnea and asthma), psychiatric conditions [17,18,20,22,26,29,32,33], and gastroesophageal reflux [11,18,29,33]. The presence of comorbidities in COPD subjects influences their clinical outcomes, demonstrated by increased frequency and severity of exacerbations, impairment in quality of life, and eventually an increased mortality [34,35]. The presence of comorbidities is essential in designing individualized treatment plans for COPD patients that enable better symptom control, better health-related quality of life, and improved survival.
1. Frequency of comorbidities in COPD
It is well known that the existence of comorbidities increases with age in the general population. However, COPD patients appear to have comorbidities earlier in life compared to non-COPD subjects [33]. Mechanisms explaining the higher frequency of comorbidities in COPD include the premature aging process, possibly due to high oxidative stress levels, reduction in endogenous antiaging molecules, and cellular senescence, among other factors [33,36].
However, accelerated aging does not explain the variability observed in the prevalence of comorbidities in different studies. For example, in the study by Schwab et al. [32] the prevalence of coronary artery disease was 19.9% among COPD patients with a mean age of 70.6 years, compared to 47.8% in the Battaglia et al.’s study [25] in patients in the same age group (mean age, 71.8 years). Other pathophysiological mechanisms may be involved in the development of comorbidities, as systemic inflammation is associated with smoking or the inhalation of noxious environmental particles. This systemic inflammation has been associated with the development of cardiovascular diseases, neoplasms, or skeletal muscle dysfuncion [37].
Variability in the prevalence of comorbidities is also probably related to the characteristics of the studied population. Some studies analyzed comorbidities in patients admitted to hospital for COPD exacerbations, while others analyzed ambulatory, and therefore, milder COPD patients. To illustrate these differences, the presence of comorbid asthma in a large administrative health claims dataset was 14.7% [26], whereas it rose to 32.5% in COPD patients from a referral hospital in South Korea [28]. In addition to the different severity of COPD, different aspects like the genetic background of the populations and different environmental exposures may partly account for the differences in the prevalence of some comorbidities [38].
The two most frequent comorbidities in COPD are hypertension and coronary artery disease, but chronic heart failure, arrhythmia, and atrial fibrillation are also among the 13 most frequent comorbidities. Therefore, it is not surprising that the main cause of death in patients with mild to moderate COPD is cardiovascular disease. The high prevalence and impact of cardiovascular comorbidity in COPD justify the systematic evaluation of cardiovascular diseases in these patients. The link between COPD and cardiovascular disease is not completely clear. They share important etiologic factors (for example, smoking) and the systemic inflammation, the lung hyperinflation, the reduced oxygenation and associated factors like sedentarism and obesity may explain the high frequency of cardiovascular comorbidities in COPD [17,34,39].
2. Impact of comorbidities in COPD
Not all comorbidities have demonstrated an association with poor outcomes in COPD patients, which may have implications for clinical practice. Divo et al. [34] developed the concept of the comorbidome taking into account the frequency and impact on mortality in a series of 78 comorbidities found in COPD patients from the BODe cohort. Among them, only 12 comorbidities were associated with increased mortality in COPD; similarly, only six of the most frequent comorbidities identified in our systematic review showed a significant association with increased mortality: coronary artery disease, diabetes, psychiatric disorders, chronic heart failure, atrial fibrillation, and other arrhythmias.
Nevertheless, other comorbidities may be associated with different outcomes in COPD. In the large longitudinal ECLIPSE study, self-reported gastroesophageal reflux was associated with an increased risk of COPD exacerbations and hospitalizations [40]. Interestedly, cardiovascular diseases, like congestive heart failure and coronary artery disease are relevantly associated with increased risk of exacerbations and hospitalizations and a prolonged length of hospital stay.
Asthma is also significantly associated with more frequent COPD exacerbations. Asthma may coexist in up to 25% of COPD patients and this correlation implies more severe respiratory symptoms, more frequent exacerbations, and significantly impaired quality of life compared with COPD alone [41-44]. It is important to recognize the coexistence of asthma because it has therapeutic implications due to inhaled corticosteroids.
The coexistence of cardiovascular disease and COPD results in a significantly impaired quality of life. This impairment may be partly due to the limited exercise capacity caused by an imbalance in the oxygen transportation, alterations in perfusion, and diffusion of the cardiopulmonary system, among other pathophysiological mechanisms [45]. The coexistence of chronic heart failure and COPD may produce severe dyspnea on exertion and it might limit performance in the daily activities [45]. Finally, these alterations may be complicated by psychological distress [46].
Despite the frequency and impact of the coexistence of chronic heart failure and COPD, some studies have demonstrated that treatment for these patients does not always follow the existing guidelines. In particular, there is a low level of prescription of cardioselective beta-blockers, which may have a negative impact on the disease progression in these patients [47,48].
3. Limitations
Therefore, the present systematic review presented important data on the most prevalent comorbidities in COPD patients and their main associations with important clinical outcomes. However, the review was based only on studies from the MEDLINE, Lilacs, and Scielo databases. This limited search strategy can lead to publication bias and decrease the likelihood of finding relevant studies.
Conclusion
Comorbidities are frequent in individuals with COPD although their prevalence varies according to patient characteristics and different study designs. Comorbidities do have a negative impact on several outcomes in COPD, including the symptoms, exercise capacity, quality of life, and survival among others. It is essential to understand the repercussions of each comorbidity in COPD, in order to design more personalized and effective treatments approaches.
Notes
Authors’ Contributions
Conceptualization: dos Santos NC, Miravitlles M, de Almeida VDC, Camelier FWR. Methodology: dos Santos NC, Camelier AA, Maciel RRBT, Camelier FWR. Formal analysis: dos Santos NC, Miravitlles M, de Almeida VDC, Camelier FWR. Data curation: dos Santos NC, Camelier AA, Maciel RRBT, Camelier FWR. Software: dos Santos NC, Maciel RRBT, Camelier FWR. Validation: Miravitlles M, de Almeida VDC, Camelier AA, Maciel RRBT, Camelier FWR. Investigation: dos Santos NC, Miravitlles M, Camelier FWR. Writing - original draft preparation: dos Santos NC, Miravitlles M, Camelier AA, de Almeida VDC, Camelier FWR. Writing - review and editing: dos Santos NC, Miravitlles M, Camelier AA, de Almeida VDC, Camelier FWR. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
No funding to declare.
Acknowledgements
We would like to thank the Stricto Sensu Graduate Program in Pharmaceutical Sciences at the State University of Bahia for all the support and partnership.
Supplementary Material
Supplementary material can be found in the journal homepage (http://www.e-trd.org).
Keywords used in the electronic search with the Boolean operators “AND” and “OR”.