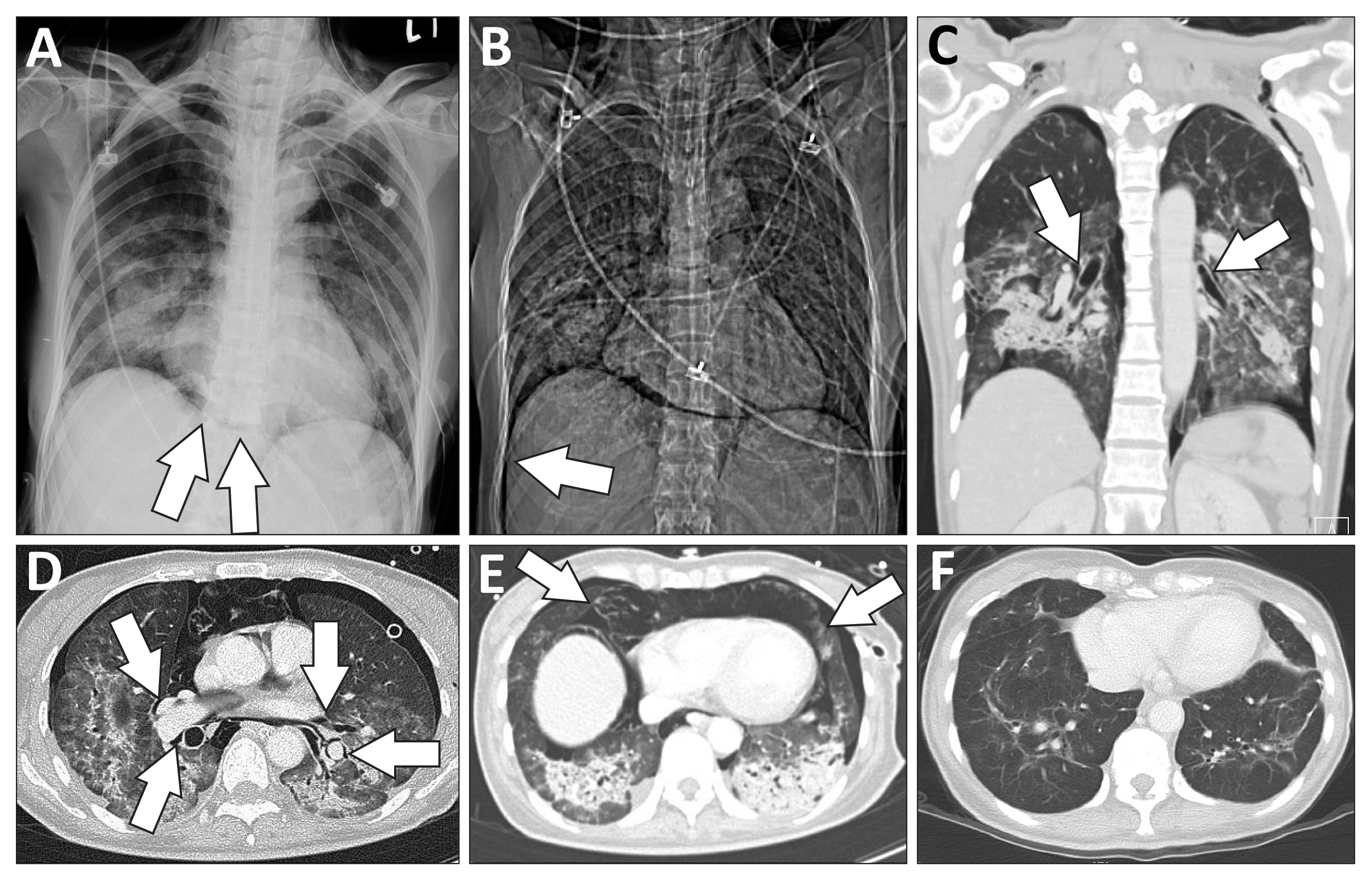
A 51-year-old woman with pneumonia received mechanical ventilation after endotracheal intubation. She developed pneumothorax, which was immediately treated by the placement of a left-side thoracostomy tube. Ethical approval was waived because there was no concern for maintaining the patient’s anonymity in the written text and radiographic images. Chest radiography revealed subcutaneous emphysema in the supraclavicular fossae and a lucent stripe outlining the base of the heart, i.e., the continuous diaphragm sign (
Fig. 1A), indicating pneumomediastinum. A computed tomography (CT) scan disclosed right pneumothorax with radiographic deep sulcus (
Fig. 1B), air dissection along the bronchovascular sheath in the perihilar area, suggesting the Macklin effect (
Fig. 1C, D), and pneumomediastinum with extensive gas collection in the pre-cardiac area (
Fig. 1E), causing cardiac compression and displacement. After inserting a right thoracostomy tube, adjusting the ventilator settings and using high oxygen concentrations, the patient recovered from barotrauma without progression to life-threatening pneumomediastinum. Finally, she was liberated from mechanical ventilation and discharged. A follow-up CT scan revealed that the heart had returned to its normal position (
Fig. 1F).
The first important finding was the CT image of pneumomediastinum with significant cardiac compression
1. The second was the compatible radiographic findings of the Macklin effect
2. In our patient, there was obvious air dissection along the peribronchial and perivascular sheaths. This may have indicated that there was increased alveolar pressure causing barotrauma with released air migrating through the bronchovascular sheath to the mediastinum, which is known as the Macklin effect
3. Hence, ventilator-induced barotrauma was likely the cause of pneumomediastinum in our case. To decrease barotrauma in this mechanically ventilated patient, the ventilator settings should be adjusted to prevent further alveolar overdistention. More importantly, the use of negative-pressure thoracostomy tube drainage may reestablish negative intra-pleural pressure and accelerate the resolution of barotrauma. As highlighted by these findings, in mechanically ventilated patients with barotrauma, pneumomediastinum should always be investigated and evaluated for cardiac compression, which warrants early management for a successful resolution.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



