Current Status of Noninvasive Ventilation Use in Korean Intensive Care Units: A Prospective Multicenter Observational Study
Article information
Abstract
Background
Data on noninvasive ventilation (NIV) use in intensive care units (ICUs) are very limited in South Korea.
Methods
A prospective observational study was performed in 20 ICUs of university-affiliated hospitals from June 2017 to February 2018. Adult patients (age>18 years) who were admitted to the ICU and received NIV treatment for acute respiratory failure were included.
Results
A total of 156 patients treated with NIV were enrolled (mean age, 71.9±11.6 years). The most common indications for NIV were acute hypercapnic respiratory failure (AHRF, n=89) and post-extubation respiratory failure (n=44). The main device for NIV was an invasive mechanical ventilator with an NIV module (61.5%), and the majority of patients (87.2%) used an oronasal mask. After the exclusion of 32 do-not-resuscitate patients, NIV success rate was 68.5% (85/124); ICU and hospital mortality rates were 8.9% and 15.3%, respectively. However, the success rate was lower in patients with de novo respiratory failure (27.3%) compared to that of patients with AHRF (72.8%) or post-extubation respiratory failure (75.0%). In multivariate analysis, immunocompromised state, de novo respiratory failure, post-NIV (2 hours) respiratory rate, NIV mode (i.e., non-pressure support ventilation mode), and the change of NIV device were significantly associated with a lower success rate of NIV.
Conclusion
AHRF and post-extubation respiratory failure were the most common indications for NIV in Korean ICUs. Overall NIV success was achieved in 68.5% of patients, with the lowest rate in patients with de novo respiratory failure.
Introduction
Noninvasive ventilation (NIV) is associated with decreased intubation and mortality rates in patients with acute exacerbation of chronic obstructive pulmonary disease (COPD)1 or cardiogenic pulmonary edema2. The treatment also plays a critical role in chronic respiratory failure of patients with a neuromuscular disease or chronic, severe and stable COPD34.
NIV has been used for various applications in clinical practice, such as to facilitate early weaning from invasive mechanical ventilation, for respiratory support after surgery5, during certain procedures6, or as palliative therapy7. The use of NIV and its success rate are increasing8910. However, the proportion of NIV use differs by region and patient condition10. In France, 39% of patients on a ventilator receive NIV11 whereas 20% of those on a ventilator in the New England region of the United States use NIV12. In Korea, one study reported that those receiving NIV accounted for 4% of all ventilated patients13.
The choice of mask is crucial for the success of NIV and it usually depends on considerations regarding patient comfort, air-leaks, and cost8. A facial (oronasal) mask is the most widely used method for patients with acute respiratory failure. However, helmets are increasingly being used in some countries8. Although NIV use was not associated with an improved outcome in patients with de novo respiratory failure, a recent study showed that helmets were associated with reduced intubation and mortality rates in these patients14.
A few small studies have been conducted on NIV use in South Korea1315 but the data are very limited. Therefore, in this multicenter study, we prospectively collected data on NIV use from patients being treated in Korean intensive care units (ICUs). We investigated the primary indications for NIV use and patient outcomes, as well as practice patterns, such as the NIV settings and type of interfaces used.
Materials and Methods
1. Study population
This was a prospective observational study performed in 20 ICUs of university-affiliated hospitals from June 1, 2017 to February 28, 2018. Adult patients (age>18 years) who were admitted to the ICUs and received NIV treatment for acute respiratory failure were prospectively enrolled. Among the indications for NIV, acute hypercapnic respiratory failure (AHRF) indicates respiratory failure in patients with chronic lung disease (obstructive or restrictive), and de novo respiratory failure usually indicates respiratory failure in patients without chronic respiratory disease, mostly those with hypoxemic respiratory failure, such as pneumonia, postoperative respiratory failure, sepsis, or acute respiratory distress syndrome (ARDS)910. In our study, we included do-not-resuscitate (DNR) patients who received NIV, and the only exclusion criterion was refusal to provide informed consent for collection of clinical data.
This study was supported by a 2017 grant from the Korea Academy of Tuberculosis and Respiratory Diseases. The ethics committees from all participating hospitals approved this study, as did the Hallym University Institutional Review Board (approval no. 2017-I044). Informed consent was obtained from all enrolled patients or their legal surrogates.
2. Data collection and outcomes
We collected patient demographic information and the following data: comorbidities, underlying lung diseases, primary indications for NIV, and mental status (Richmond Agitation Sedation Score [RASS]) and severity of illness (Sequential Organ Failure Assessment [SOFA]) immediately before starting NIV. We also assessed arterial blood gas analyses, as well as vital signs, before and 2 hours after NIV was started. We investigated the type of NIV machine (i.e., invasive mechanical ventilator [MV] with NIV module, invasive MV without NIV module, dedicated NIV ventilator, or home MV), the interfaces (i.e., oronasal, nasal or total facial masks, nasal pillow, or helmet), and the circuits (i.e., double limb circuit, single limb circuit with leak port, or single limb circuit with exhalation valve). We also investigated the NIV settings (main NIV modes, fractional inspired oxygen [FiO2], inspiratory positive airway pressure [IPAP], expiratory positive airway pressure [EPAP], and estimated tidal volume) and their mean durations (hours/day).
After the exclusion of DNR patients, treatment success and failure, complications from NIV treatment, and ICU and hospital mortality rates were investigated as patient outcomes. Treatment success included successful weaning from NIV and successful transfer to the general ward in a stable condition with the NIV device in place. Treatment failure included (1) intubation and invasive MV, (2) tracheostomy, and (3) hopeless discharge with NIV device. Patients who died within 24 hours of NIV weaning were also classified as NIV failures. A large leak was defined when leak flow was >60 L/min, or when the attending doctor considered it too large to allow the treatment continue.
The primary outcomes in this study were the NIV success rate and the common indications for NIV treatment in Korean ICUs. Secondary outcomes were the NIV settings, type of machine and interfaces used, and reasons for NIV failure.
3. Statistical analysis
In this study, descriptive analyses were primarily performed, because we were interested in the current status of NIV use. All categorical variables are presented as numbers with percentages, and all continuous variables are presented as means with standard deviations. Student's t test was used to compare continuous variables, and the chi-square or Fisher exact test was used to compare categorical variables. Logistic regression analysis was performed using covariates with a p-value of <0.10 on univariate analysis to identify independent factors for NIV success (and hospital survival); we employed a backward stepwise selection method based on the likelihood ratio. IBM SPSS for Windows software ver. 22.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses. A p-value of <0.05 was considered significant.
Results
1. Study population and baseline characteristics
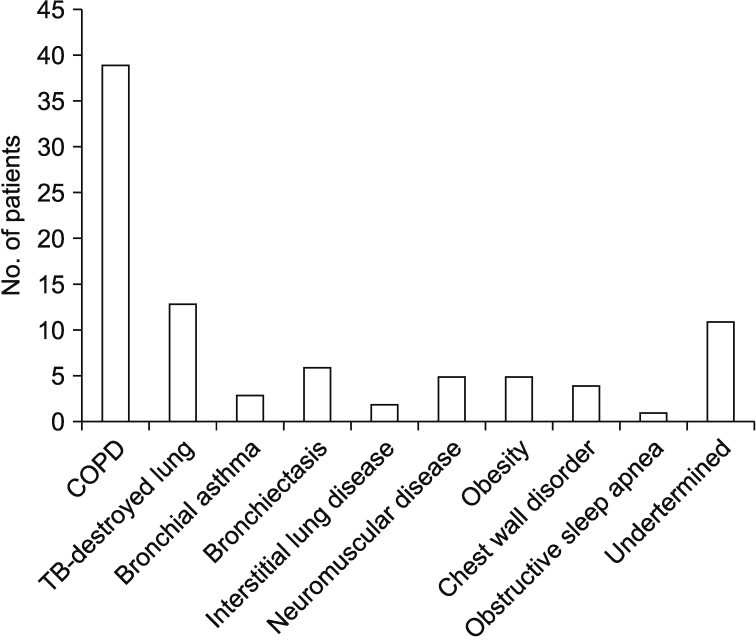
A total of 168 patients treated with NIV were initially screened from 20 ICUs during the study period. Twelve patients refused to consent, and 156 were finally enrolled in the present study (Figure 1). The mean age was 71.9±11.6 years and the mean body mass index was 21.6±5.3 kg/m2. Diabetes (n=39) and hypertension (n=62) were the most common comorbidities. Of all patients, 118 (75.6%) had underlying lung disease, with COPD (n=60) and tuberculosis-destroyed lung (n=18) being the most common (Table 1). One hundred and forty-three patients (91.7%) started NIV in the ICU and 13 started NIV in other places; 10 in general ward, one in emergency department, and two in other locations. The most common cause for starting NIV was AHRF (n=89, 57.1%) (Figures 1, 2), followed by post-extubation respiratory failure (n=44, 28.2%). Of all patients, 59 (37.8%) started high flow nasal cannula (HFNC) before NIV. At the time that NIV was started, the mean SOFA score was 4.2±2.7 and the median RASS was 0.0 (−1.0 to 0.0). Thirty-two DNR patients (20.5%) were included in this study.
2. NIV treatments (devices, modes, settings, and duration)
Invasive MV with the NIV module was used in 96 patients (61.5%), and invasive MV without the NIV module was used in two patients (1.3%); a dedicated NIV machine (ICU use) was used in 33 patients (21.2%), and a home MV was used by 25 patients (16.0%). The dedicated NIV machine was most commonly used in patients with AHRF (57.6%, 19/33). Among the NIV modes used, the pressure support ventilation (PSV, n=66) and spontaneous/time (ST, n=48) modes were the most commonly used; pressure-controlled ventilation in 36, volume controlled ventilation in two, continuous positive airway pressure in two, and averaged volume-assured pressure support in two patients. The mean IPAP and EPAP values were 14.5±3.8 and 5.0±1.5 cm H2O, respectively, and the estimated tidal volume was 499.6±198.3 ml. Daily NIV duration was 14.5 hours (6.0–22.0 hours), and total time on NIV was 3.0 days (1.0–6.0 days). Of all patients, 26 (16.7%) received a sedative (or analgesic) during NIV treatment; remifentanil (n=15) and dexmedetomidine (n=8) were the most commonly used. The NIV device was changed to another device in 27 patients (17.3%).
3. Interfaces
Among the interfaces used in this study, oronasal mask was the most commonly used (n=136, 87.2%), followed by a helmet (n=12), a nasal mask (n=4), a nasal pillow (n=3), and a total facial mask (n=1). Patients with AHRF, and those with post-extubation respiratory failure, used oronasal masks most frequently (91.0% and 84.1%, respectively). Among the circuit types used, a double limb circuit (n=99) was most commonly used, while a single limb circuit with a leak port was used in 52 patients; a single limb circuit with exhalation valve was used by five patients. At least one mask change for any reason occurred during the treatment of 29 patients (18.6%). Among the 12 patients with helmet, five patients used a helmet for post-extubation respiratory failure and four patients used it for AHRF; three patients for de novo respiratory failure. The most common mode used for helmet was PSV and pressure-controlled ventilation (n=7 and n=3, respectively), and after the exclusion of two DNR patients, NIV success was achieved in eight patients (80.0%).
4. Complications
Complications of NIV were reported in 32 patients (20.5%), with skin erythema (n=26) being the most frequent. Other complications included abdominal distension (n=7), dry mouth (n=6), aspiration (n=5), claustrophobia (n=4), nasal congestion or sinus pain (n=1), and mucus plugs (n=1).
5. NIV outcomes
Among 124 patients, NIV success was achieved in 85 (68.5%) patients; 57 patients were successfully weaned from NIV, and 28 were stabilized and transferred to the general ward on an NIV machine. Among the different indications, the NIV success rate was lower for de novo respiratory failure (27.3%) compared to that for AHRF (72.8%) or post-extubation respiratory failure (75.0%) (Figure 3). Thirty-nine patients did not respond to NIV (i.e., treatment failure). Among them, 30 patients were intubated and conventionally ventilated, and six underwent tracheostomy (hopeless discharge with NIV in place, n=3). The reasons for NIV failure are shown in Table 2.

Primary indications for NIV (n=124). AHRF: acute hypercapnic respiratory failure; RF: respiratory failure; CPE: cardiogenic pulmonary edema; NIV: noninvasive ventilation.
6. Factors associated with NIV success and hospital survival
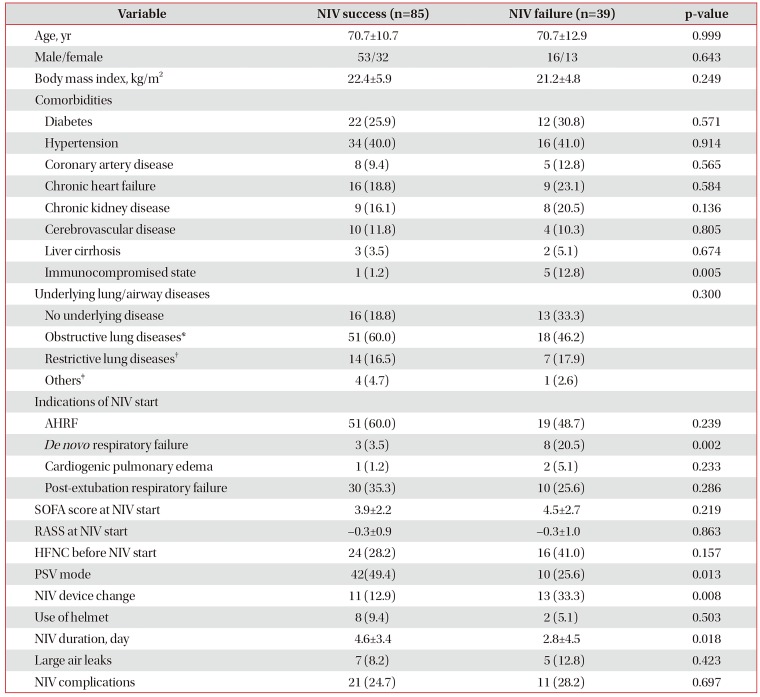
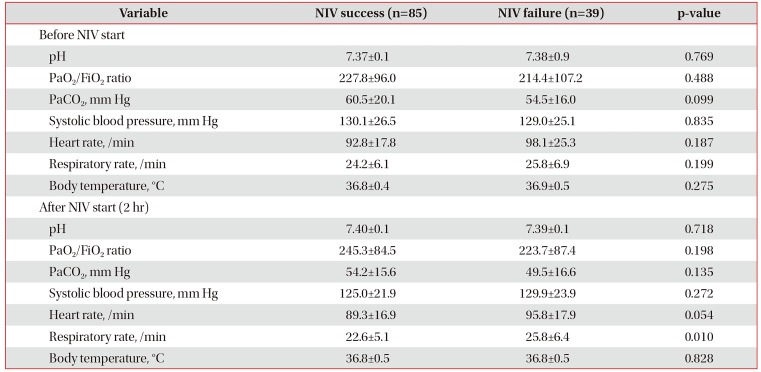
Univariate analyses revealed that eight variables (i.e., immunocompromised state, de novo respiratory failure, non-PSV mode, NIV device change, NIV duration, pre-NIV PaCO2, post-NIV heart rate, and post-NIV respiratory rate) (Tables 3, 4) were associated with NIV success, with a p-value of <0.100. In multivariate analysis, where age and gender were included, immunocompromised state, de novo respiratory failure, non-PSV mode, NIV device change, and a high post-NIV respiratory rate were significantly associated with a low success rate of NIV (Table 5).

Comparisons in baseline and clinical parameters between patients with NIV success and patients with NIV failure (n=124)

Comparisons in vital signs and arterial blood gas results between patients with NIV success and patients with NIV failure (n=124)
Regarding hospital survival, seven variables (age, sex, SOFA score at NIV start, post-NIV heart rate, post-NIV respiratory rate, length of ICU stay, and NIV success) were selected from univariate analyses. Among them, NIV success was significantly associated with hospital survival in multivariate analysis (Table 5).
Discussion
This is the first prospective study on current NIV use in Korean ICUs, and patients from 20 university-affiliated hospitals across the nation were included. Our study had several main findings. First, the most common indications for starting NIV were AHRF (57.1%) and post-extubation respiratory failure (28.2%); the proportion of patients using NIV for de novo respiratory failure was lower (11.5%). Second, NIV success was achieved in 68.5% of patients, and de novo respiratory failure had a relatively low success rate among the NIV indications. Third, the main device for NIV was the invasive MV with the NIV module (61.5%), and the majority of patients (87.2%) used an oronasal mask.
The rate of NIV use varies by country and hospital, but recent studies have reported an increase in the rate of NIV use. Overall NIV use in a French study increased to 37% in 2010–2011, compared to 16% (1997) and 28% (2002) during earlier periods9. In Spain, the NIV use rate increased from 0.4 per 100,000 (1997) to 15.1 per 100,000 hospitalized patients (2010), in contrast to a decrease in the use of invasive MV16. In a regional survey of North America, 20% of ventilated patients received NIV, with the rate ranging from 0% to 55% among different hospitals12. In particular, NIV was started most often in the emergency department in some regions17, which was in contrast to our study where only one patient started NIV in the emergency department.
The most common indications for NIV have been acute exacerbation of COPD and cardiogenic pulmonary edema; in French studies, they accounted for >40% and >20%, respectively, of NIV indications89101217. These results could be due to proven efficacy in randomized controlled trials12. The current guidelines still strongly recommend NIV for these patient groups18. In our study, AHRF was the most common indication, followed by post-extubation respiratory failure and de novo hypoxemia. A European survey reported that post-extubation respiratory failure was the second most common indication in Germany and the United Kingdom8, and a recent French study also demonstrated a substantial increase in NIV use in this population9. Based on previous multicenter randomized studies, NIV may reduce re-intubation and mortality rates when applied immediately after planned extubation in selected patients at high-risk for respiratory failure1920. However, NIV is not recommended in patients without COPD and with established post-extubation respiratory failure18.
In our study, the proportion of NIV use for de novo respiratory failure was lower compared to other indications (i.e., AHRF and post-extubation respiratory failure), in keeping with previous studies911, but the NIV failure rate was higher. Although NIV could be beneficial in selected patients, insufficient evidence supports its use for de novo respiratory failure18. Particularly, NIV failure in this group was associated with a higher mortality rate compared to first-line invasive ventilation21. The effect of NIV on reducing the work of breathing remains uncertain22 and high transpulmonary pressure may aggravate lung injury23. However, HFNC may be promising in selected patients with de novo respiratory failure2425. In our study, 11 patients (61.1%) with de novo respiratory failure received HFNC before NIV.
The invasive MV with the NIV module was used in 61.5% of patients, similar to the rate in France. However, in other countries, the use of a dedicated NIV ventilator was more frequent (41.2% in the United Kingdom and 37.5% in Germany)8. Although the frequencies differed by hospital and country, it is important that physicians are aware that asynchrony can occur more frequently among invasive MVs26, and many invasive MVs may need to be adjusted if a large leak occurs27. Among NIV modes, pressure support modes (PSV and ST) were the most widely used in our study, but the applied levels of pressure support and positive end expiratory pressure (PEEP) were not different from other studies.
The oronasal mask was the most commonly used (87.2%) device, similar to data from other countries81012; helmets were used by 12 patients (7.7%). A European survey reported that helmets were used in <10% of patients, whereas 29.9% of Italian patients with ARDS used helmets28. Reports on the effects of NIV on patients with ARDS are conflicting. However, based on recent studies, NIV (via helmet) might be beneficial in these populations once optimal PEEP levels with less leakage have been obtained via interfaces1429.
In a regional survey conducted in the United States, the estimated success rate was 51.1%, and the NIV success rate increased from 56.0% (2002) to 70.0% (2010/2011) in France. Although the NIV success rate (68.5%) was not markedly higher in our study compared to other investigations, the daily NIV duration was longer at 14.5 hours (6.0–22.0 hours). However, we did not investigate patients who prematurely discontinued NIV and survived without intubation, but we classified patients who became clinically stable and were transferred to the general ward with a NIV device as the NIV success group. This finding should be considered when our results are interpreted.
These days, NIV use and its success rates are increasing. In particular, the survival rate in those receiving NIV for de novo respiratory failure has increased in France. This may be because of trends toward better patient selection and greater proficiency of physicians9. However, given the substantial complication and treatment failure rates of NIV, physician experience and adequate staff training seem to be crucial1230.
Several limitations to our study should be mentioned. First, we could not investigate trends in overall NIV use or the distribution of NIV indications over time. In particular, data on the NIV use during spring time were not investigated in this study. Second, we did not include patients who received NIV outside the ICU, so it is possible that NIV use in the hospitals may have been underestimated. Third, the criteria for starting NIV may have differed among hospitals. However, we were interested in the current practices of NIV use in Korean ICUs. Finally, we could not involve all ICUs in Korea, and the number of patients enrolled in this study was not large enough to draw a definite conclusion. Hence, further large-scale studies will be needed in the future.
In conclusion, our study revealed that the most common indications for starting NIV were AHRF and post-extubation respiratory failure in Korean ICUs, and the overall NIV success rate was 68.5%. Although the proportion of patients receiving NIV for de novo respiratory failure was lower, their failure rate was higher compared to other indications. Future comprehensive studies on overall trends in NIV use and its indications, as well as on factors affecting NIV outcomes, are needed.
Acknowledgments
This work was supported by a 2017 research grant from the Korea Academy of Tuberculosis and Respiratory Disease. The funders had no role in study design, data collection and analysis, preparation. We thank the following investigators for the participation in this study: Jin Woo Kim (The Catholic University of Korea, Uijeongbu St. Mary's Hospital), Jong Hoo Lee (Jeju National University Hospital), Tae Oak Kim (Chonnam National University Hospital), Yun Mi Sin (Chungbuk National University), and Jik Hwan Ha (The Catholic University of Korea, Incheon St. Mary's Hospital).
Notes
Authors' Contributions:
Conceptualization: Nam H, Cho JH, Choi EY, Chang Y, Hwang JJ, Sim YS, Park S.
Methodology: Sim YS, Moon JY, Lee K, Choi WI, Hwang JJ, Park SY, Park TS, Kim SW, Kang HK, Park S.
Formal analysis: Nam H, Choi EY, Chang Y, Park TS, Moon JY, Park SY, Kim SW, Kang HK, Park S.
Writing - original draft preparation: Nam H, Cho JH, Choi WI, Lee K, Park S.
Writing - review and editing: Nam H, Cho JH, Choi EY, Chang Y, Choi WI, Hwang JJ, Moon JY, Lee K, Kim SW, Kang HK, Sim YS, Park TS, Park SY, Park S.
Approval of final manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.