Primary Malignant Fibrous Histiocytoma of the Chest Wall Misdiagnosed as Traumatic Hemothorax
Article information
Abstract
Malignant fibrous histiocytoma (MFH), a type of sarcoma, is a malignant neoplasm with uncertain origins that arise from both the soft tissues and the bone. The occurrence of MFH on the chest wall is extremely rare. We hereby report a case of a 72-year-old woman who was incidentally detected with MFH after a traffic accident.
Introduction
Malignant fibrous histiocytoma (MFH) is the most common malignant soft tissue tumor. MFH occurs most commonly in the extremities (70-75%), followed the trunk and retroperitoneum. It is a frequently occurring soft tissue tumor with aggressive biological behavior. Primary MFH of the chest wall is especially rare.
We report a case of a 72-year-old woman in whom MFH was detected incidentally after she had a traffic accident. We describe this unusual case and review the literature.
Case Report
A 72-year-old woman complained of right-sided chest pain and orthopnea following a traffic accident that occurred 1 month previously. Chest radiography and computed tomography revealed large amounts of right pleural effusion and a pathological seventh rib fracture (Figure 1). A hemorrhagic fluid was aspirated at thoracentesis. She was then diagnosed with traumatic hemothorax and a closed thoracostomy was performed. Laboratory examination of the pleural effusion revealed that it was exudative, and had an adenosine deaminase level of 15.7 IU/L, white blood cell count of 980/mm3 (lymphocyte count 80%), and red blood cell count of 6,560/mm3. Except for the level of tumor marker cancer antigen-125, the levels of tumor markers such as carcinoembryonic antigen and cytokeratin fragment 19 remained within the normal range. After drainage of 1.5 L, the symptoms improved.

Chest radiographs showing large amounts of pleural effusion and a fracture in the seventh right rib.
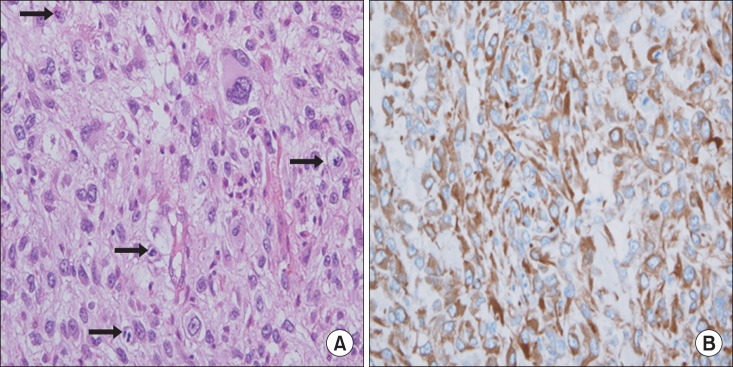
Chest radiography performed 7 days after closed thoracostomy revealed a large amount of the remaining pleural effusion (Figure 2). We then performed video-assisted thoracoscopic surgery for the persistent retained hemothorax. However, lung decortication and rib resection had to be performed because of the presence of a very large mass at the incision site (Figure 3). Histopathological examination of the biopsy specimen revealed marked cytological and nuclear pleomorphism with frequent mitoses. The tumor cells stained positive for vimentin only (Figure 4). The mass on the chest wall and pleura was confirmed as a pleomorphic MFH. Thus, pleomorphic MFH was initially misdiagnosed as traumatic hemothorax.

(A) Chest radiograph showing the remaining pleural effusion in the right thoracic cavity 7 days after performing the closed thoracostomy. (B) Chest computed tomography scans showing remaining pleural effusions after closed thoracostomy.
Discussion
MFH is among the most common soft-tissue sarcomas in adults (20-30%), and is principally located in the extremities or the retroperitoneum1. In a retrospective series of 167 cases reported by Kearney et al.2, 51% arose in the lower limbs, 24% in the upper limbs, 16% in the trunk, and 9% retroperitoneum. The chest wall is a rare site of origin3.
The peak incidence is in the fifth decade of life, with a predominance of elderly male patients. There is no typical clinical symptom, but the patients with MFH of the chest wall usually experience chest pain, cough, and hemoptysis. However, there were no pre-trauma tumor-related symptoms in our case. In our case, MFH was diagnosed by pleural effusion. Because the majority of the data available in the literature are case reports due to the low frequency of the diseases, the frequency of presence of pleural effusion with MFH is unknown.
The mass was not seen because of large amount of pleural effusion in our case, however, the important diagnostic tool is chest computerized tomography (CT) and magnetic resonance (MR) imaging. The mass usually shows intense enhancement on CT with a clear margin separating it from the surrounding tissue4. Furthermore, the mass often shows decreased central attenuation due to necrosis, hemorrhage and mucoid material5. On MR imaging, the mass shows an intermediate to low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, which frequently shows inhomogeneous central intensity6. The final diagnosis was confirmed by results of the histopathology and immunohistochemistry. Immunohistochemical staining for various molecules such as caletinin, CD68, pan-cytokeratin, vimentin were performed to rule out other malignancies.
Wide resection is the first choice treatment for all soft-tissue sarcomas. The mean survival of patients without operation is 11.7 months, those of patients whom underwent operation is 23.2 months7,8,9,10. The additional chemotherapy and radiotherapy may play a role in treating osseous MFH. The tumor grade, size, and the presence of distant metastases at the initial presentation remain the most important prognostic factor for MFH11,12. Favorable factors of MFH was Union for International Cancer Control/American Joint Committee on Cancer (UICC/AJCC) stage I and II, superficial location, myxoid type and under 50 years, supporting the rational for radical en-block resection of tumor tissues.
In conclusion, primary MFH of the chest wall is extremely rare tumor and surgery is treatment of choice of MFH. We report a case of a 72-year-old woman in whom MFH was detected incidentally after she had a traffic accident.
Acknowledgements
This study was supported by a grant from Wonkwang University in 2012.
Notes
No potential conflict of interest relevant to this article was reported.