 |
 |
| Tuberc Respir Dis > Volume 84(1); 2021 > Article |
|
Abstract
Background
Methods
Results
Notes
Authors’ Contributions
Conceptualization: Kang Y, Mok J. Methodology: Kang Y, Mok J. Formal analysis: Kang Y, Lee K, Kim KU, Park HK, Lee MK, Mok J. Data curation: Kang Y, Jo EJ, Eom JS, Kim MH, Mok J. Writing - original draft preparation: Kang Y, Mok J. Writing - review and editing: Kang Y, Jo EJ, Eom JS, Kim MH, Lee K, Kim KU, Park HK, Lee MK, Mok J. Approval of final manuscript: all authors.
Figure 1.
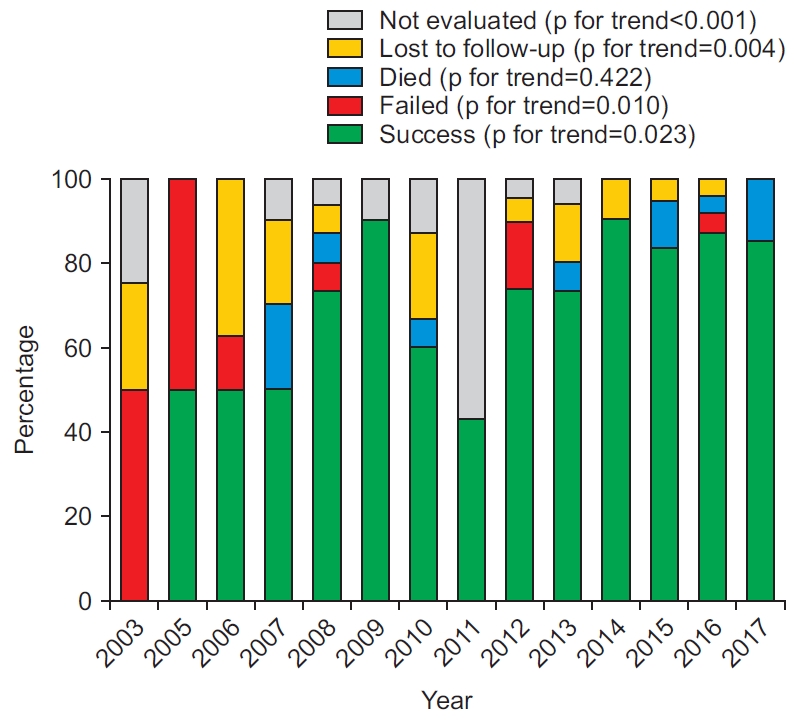
Table 1.
| Characteristic | Total (n=176) | Pre-PPM period (n=64) | Post-PPM period (n=112) | p-value* |
|---|---|---|---|---|
| Age, yr | 45.0 (31.0-58.0) | 41.0 (29.3-55.8) | 47.5 (35.3-62.8) | 0.027 |
| Male sex | 108 (61.4) | 37 (57.8) | 71 (63.4) | 0.465 |
| BMI, kg/m2 | 21.2 (19.3-23.1) | 20.8 (19.5-22.7) | 21.4 (19.2-23.3) | 0.427 |
| HIV positivity | 1 (0.6) | 1 (1.6) | 0 (0) | 0.364 |
| Comorbidities | ||||
| Diabetes mellitus | 41 (23.3) | 19 (29.7) | 22 (19.6) | 0.129 |
| Malignancy | 22 (12.5) | 9 (14.1) | 13 (11.6) | 0.636 |
| Chronic liver disease | 12 (6.8) | 4 (6.3) | 8 (7.1) | >0.999 |
| Chronic lung disease | 10 (5.7) | 2 (3.1) | 8 (7.1) | 0.331 |
| Cardiovascular disease | 10 (5.7) | 1 (1.6) | 9 (8.0) | 0.096 |
| Chronic kidney disease | 8 (4.5) | 2 (3.1) | 6 (5.4) | 0.712 |
| Ever-smoker | 81 (46.0) | 27 (42.2) | 54 (48.2) | 0.440 |
| Previous TB treatment | 91 (51.7) | 44 (68.8) | 47 (42.0) | 0.001 |
| Additional extra-pulmonary TB | 10 (5.7) | 4 (6.3) | 6 (5.4) | >0.999 |
| Initial, sputum AFB smear positive | 128 (72.7) | 58 (90.6) | 70 (62.5) | <0.001 |
| Radiological findings | ||||
| Cavities | 114 (64.8) | 44 (68.8) | 70 (62.5) | 0.404 |
| Bilateral lung involvement | 86 (48.9) | 35 (54.7) | 51 (45.5) | 0.243 |
| Laboratory findings | ||||
| Serum albumin, g/dL | 4.1 (3.6-4.4) | 3.9 (3.5-4.4) | 4.2 (3.8-4.5) | 0.019 |
| Serum total cholesterol, mg/dL† | 165.0 (140.0-187.0) | 166.0 (136.3-186.0) | 165.0 (147.0-192.0) | 0.584 |
| Diagnostic modality | ||||
| LPA for isoniazid and rifampicin | 68 (38.6) | 5 (7.8) | 63 (56.3) | <0.001 |
| Xpert MTB/RIF assay | 59 (33.5) | 0 (0) | 59 (52.7) | <0.001 |
| Bronchoscopy | 62 (35.2) | 29 (45.3) | 33 (29.5) | 0.034 |
Table 2.
| Variable | Total (n=176) | Pre-PPM period (n=64) | Post-PPM period (n=112) | p-value* |
|---|---|---|---|---|
| Resistance on phenotypic DST† | ||||
| Isoniazid | 165/176 (93.8) | 62/64 (96.9) | 103/112 (92.0) | 0.332 |
| Rifampicin‡ | 171/176 (97.2) | 64/64 (100) | 107/112 (95.5) | 0.160 |
| Rifabutin | 128/176 (72.7) | 49/64 (76.6) | 79/112 (70.5) | 0.388 |
| Ethambutol | 112/176 (63.6) | 39/64 (60.9) | 73/112 (65.2) | 0.574 |
| Pyrazinamide§ | 71/176 (40.3) | 30/64 (46.9) | 41/112 (36.6) | 0.182 |
| Ofloxacin | 47/176 (26.7) | 14/64 (21.9) | 33/112 (29.5) | 0.274 |
| Levofloxacin | 31/141 (22.0) | 4/29 (13.8) | 27/112 (24.1) | 0.232 |
| Moxifloxacin | 30/176 (17.0) | 7/64 (10.9) | 23/112 (20.5) | 0.103 |
| Streptomycin | 48/176 (27.3) | 13/64 (20.3) | 35/112 (31.3) | 0.117 |
| Amikacin | 23/158 (14.6) | 8/46 (17.4) | 15/112 (13.4) | 0.517 |
| Kanamycin | 36/176 (20.5) | 18/64 (28.1) | 18/112 (16.1) | 0.057 |
| Capreomycin | 25/176 (14.2) | 10/64 (15.6) | 15/112 (13.4) | 0.683 |
| Prothionamide | 30/176 (17.0) | 10/64 (15.6) | 20/112 (17.9) | 0.705 |
| Cycloserine | 18/176 (10.2) | 8/64 (12.5) | 10/112 (8.9) | 0.452 |
| Para-aminosalicylic acid | 55/176 (31.3) | 19/64 (29.7) | 36/112 (32.1) | 0.735 |
| No. of resistant drugs | 5.0 (3.0-8.0) | 5.0 (3.3-8.0) | 4.5 (3.0-8.0) | 0.657 |
| Resistance level | ||||
| MDR-TB‖¶ | 111 (63.1) | 38 (59.4) | 73 (65.2) | 0.443 |
| Pre-XDR-TB with FQ resistance** | 27 (15.3) | 7 (10.9) | 20 (17.9) | 0.220 |
| Pre-XDR-TB with SLID resistance†† | 18 (10.2) | 12 (18.8) | 6 (5.4) | 0.005 |
| XDR-TB | 20 (11.4) | 7 (10.9) | 13 (11.6) | 0.893 |
‖ Including 10 patients with rifampicin-monoresistant TB (two in the pre-PPM period; eight in the post-PPM period).
¶ Multidrug-resistant tuberculosis without additional resistance to fluoroquinolone or a second-line injectable drug.
** Multidrug-resistant tuberculosis resistant to any fluoroquinolone but not to any second-line injectable drug (amikacin, kanamycin, or capreomycin).
Table 3.
| Variable | Total (n=176) | Pre-PPM period (n=64) | Post-PPM period (n=112) | p-value* |
|---|---|---|---|---|
| Anti-TB drugs used for ≥1 mo | ||||
| Isoniazid | 14 (8.0) | 9 (14.1) | 5 (4.5) | 0.024 |
| Rifabutin | 10 (5.7) | 5 (7.8) | 5 (4.5) | 0.500 |
| Ethambutol | 34 (19.3) | 20 (31.3) | 14 (12.5) | 0.002 |
| Pyrazinamide | 116 (65.9) | 30 (46.9) | 86 (76.8) | <0.001 |
| Ofloxacin | 4 (2.3) | 4 (6.3) | 0 (0) | 0.016 |
| Levofloxacin | 64 (36.4) | 21 (32.8) | 43 (38.4) | 0.459 |
| Moxifloxacin | 90 (51.1) | 42 (65.6) | 48 (42.9) | 0.004 |
| Any fluoroquinolone† | 152 (86.4) | 62 (96.9) | 90 (80.4) | 0.002 |
| Streptomycin | 52 (29.5) | 35 (54.7) | 17 (15.2) | <0.001 |
| Amikacin | 41 (23.3) | 1 (1.6) | 40 (35.7) | <0.001 |
| Kanamycin | 56 (31.8) | 15 (23.4) | 41 (36.6) | 0.071 |
| Any injectable drug‡ | 143 (81.3) | 48 (75.0) | 95 (84.8) | 0.108 |
| Prothionamide | 141 (80.1) | 54 (84.4) | 87 (77.7) | 0.284 |
| Cycloserine | 149 (84.7) | 58 (90.6) | 91 (81.3) | 0.097 |
| Para-aminosalicylic acid | 71 (40.3) | 39 (60.9) | 32 (28.6) | <0.001 |
| Linezolid | 34 (19.3) | 3 (4.7) | 31 (27.7) | <0.001 |
| Clofazimine | 9 (5.1) | 0 (0) | 9 (8.0) | 0.027 |
| Bedaquiline | 15 (8.5) | 0 (0) | 15 (13.4) | 0.002 |
| Delamanid | 18 (10.2) | 0 (0) | 18 (16.1) | <0.001 |
| No. of drugs used for ≥1 mo | 5.0 (5.0-6.0) | 5.0 (5.0-6.0) | 5.0 (5.0-6.0) | 0.255 |
| Surgery to treat TB | 10 (5.7) | 5 (7.8) | 5 (4.5) | 0.500 |
| Total treatment duration, day | 609.0 (499.8-706.8) | 696.5 (486.0-802.8) | 608.5 (516.5-625.8) | 0.001 |
Table 4.
| Variable | Total | Pre-PPM period | Post-PPM period | p-value* |
|---|---|---|---|---|
| Total | 176 | 64 | 112 | |
| Treatment success | 128 (72.7) | 39 (60.9) | 89 (79.5) | 0.008 |
| Treatment failed | 9 (5.1) | 5 (7.8) | 4 (3.6) | 0.289 |
| Died | 11 (6.3) | 4 (6.3) | 7 (6.3) | >0.999 |
| Lost to follow-up | 16 (9.1) | 10 (15.6) | 6 (5.4) | 0.023 |
| Not evaluated | 12 (6.8) | 6 (9.4) | 6 (5.4) | 0.358 |
| MDR-TB†‡ | 111 | 38 | 73 | |
| Treatment success | 85 (76.6) | 25 (65.8) | 60 (82.2) | 0.053 |
| Treatment failed | 5 (4.5) | 3 (7.9) | 2 (2.7) | 0.336 |
| Died | 7 (6.3) | 2 (5.3) | 5 (6.8) | >0.999 |
| Lost to follow-up | 9 (8.1) | 5 (13.2) | 4 (5.5) | 0.270 |
| Not evaluated | 5 (4.5) | 3 (7.9) | 2 (2.7) | 0.336 |
| Pre-XDR§- or XDR-TB | 65 | 26 | 39 | |
| Treatment success | 43 (66.2) | 14 (53.8) | 29 (74.4) | 0.087 |
| Treatment failed | 4 (6.2) | 2 (7.7) | 2 (5.1) | >0.999 |
| Died | 4 (6.2) | 2 (7.7) | 2 (5.1) | >0.999 |
| Lost to follow-up | 7 (10.8) | 5 (19.2) | 2 (5.1) | 0.106 |
| Not evaluated | 7 (10.8) | 3 (11.5) | 4 (10.3) | >0.999 |
† Including ten patients with rifampicin-monoresistant TB (two patients in the pre-PPM period; eight in the post-PPM period).
‡ Multidrug-resistant tuberculosis without additional resistance to fluoroquinolone or a secondline injectable drug.
Table 5.
| Variable | Total (n=176) | Treatment success (n=128) | Unfavorable outcome (n=48) | p-value* |
|---|---|---|---|---|
| Age, yr | 45.0 (31.0-58.0) | 43.0 (31.0-55.8) | 51.5 (30.3-68.8) | 0.105 |
| Male sex | 108 (61.4) | 75 (58.6) | 33 (68.8) | 0.218 |
| BMI, kg/m2 | 21.2 (19.3-23.1) | 21.5 (19.5-23.3) | 20.3 (17.9-22.3) | 0.017 |
| Comorbidities | ||||
| Diabetes mellitus | 41 (23.3) | 26 (20.3) | 15 (31.3) | 0.126 |
| Malignancy | 22 (12.5) | 14 (10.9) | 8 (16.7) | 0.306 |
| Previous TB treatment | 91 (51.7) | 57 (44.5) | 34 (70.8) | 0.002 |
| Initial, sputum AFB smear positive | 128 (72.7) | 89 (69.5) | 39 (81.3) | 0.120 |
| Radiological findings | ||||
| Cavities | 114 (64.8) | 80 (62.5) | 34 (70.8) | 0.303 |
| Bilateral lung involvement | 86 (48.9) | 52 (40.6) | 34 (70.8) | < 0.001 |
| Laboratory findings | ||||
| Serum albumin, g/dL | 4.1 (3.6-4.4) | 4.2 (3.8-4.4) | 3.9 (3.4-4.4) | 0.026 |
| Serum total cholesterol, mg/dL† | 165.0 (140.0-187.0) | 167.0 (147.8-186.3) | 164.0 (133.5-189.5) | 0.372 |
| No. of resistant drugs | 5.0 (3.0-8.0) | 4.0 (3.0-8.0) | 5.0 (3.0-8.8) | 0.197 |
| Pre-XDR‡- or XDR-TB | 65 (36.9) | 43 (33.6) | 22 (45.8) | 0.134 |
| Total treatment duration, day | 609.0 (499.8-706.8) | 618.5 (607.0-723.0) | 296.0 (134.5-544.3) | <0.001 |
| Anti-TB drugs used for ≥1 mo | ||||
| Levofloxacin or moxifloxacin | 151 (85.8) | 109 (85.2) | 42 (87.5) | 0.692 |
| Any injectable drug§ | 143 (81.3) | 106 (82.8) | 37 (77.1) | 0.386 |
| Linezolid | 34 (19.3) | 28 (21.9) | 6 (12.5) | 0.161 |
| Bedaquiline or delamanid | 30 (17.0) | 25 (19.5) | 5 (10.4) | 0.152 |
| No. of drugs used for ≥1 mo | 5.0 (5.0-6.0) | 5.0 (5.0-6.0) | 5.0 (5.0-6.0) | 0.541 |
| Surgery to treat TB | 10 (5.7) | 8 (6.3) | 2 (4.2) | 0.730 |
Table 6.
| Variable |
Univariate analysis |
Multivariate analysis |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Age ≥65 yr | 0.322 | 0.142-0.734 | 0.007 | 0.189 | 0.070-0.513 | 0.001 |
| Male sex | 0.643 | 0.318-1.301 | 0.220 | - | - | - |
| BMI ≤18.5 kg/m2 | 0.407 | 0.188-0.884 | 0.023 | 0.312 | 0.127-0.766 | 0.011 |
| Diabetes mellitus | 0.561 | 0.266-1.184 | 0.129 | 0.657 | 0.270-1.595 | 0.353 |
| Previous TB treatment | 0.331 | 0.162-0.675 | 0.002 | 0.388 | 0.172-0.876 | 0.023 |
| Cavities | 0.686 | 0.335-1.407 | 0.304 | - | - | - |
| Bilateral lung involvement | 0.282 | 0.138-0.576 | 0.001 | 0.328 | 0.148-0.728 | 0.006 |
| Initial, sputum AFB smear positive | 0.527 | 0.233-1.192 | 0.124 | 1.256 | 0.455-3.468 | 0.660 |
| Serum albumin ≤3.4 g/dL | 0.310 | 0.128-0.751 | 0.009 | 0.722 | 0.237-2.200 | 0.567 |
| Pre-XDR*- or XDR-TB | 0.598 | 0.304-1.175 | 0.136 | 0.340 | 0.147-0.783 | 0.011 |
| Linezolid use ≥1 mo | 1.960 | 0.756-5.081 | 0.166 | 2.921 | 0.662-12.886 | 0.157 |
| Bedaquiline or delamanid use ≥1 mo | 2.087 | 0.750-5.812 | 0.159 | 5.939 | 1.680-20.991 | 0.006 |
References
-
METRICS

- ORCID iDs
-
Yewon Kang

https://orcid.org/0000-0002-7068-313XJeongha Mok

https://orcid.org/0000-0001-7406-1373 - Funding Information
-
Pusan National University Hospital
https://doi.org/10.13039/501100008130 - Related articles


 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



