Diffuse Hypertrophic Pachymeningeal Tuberculosis
Article information
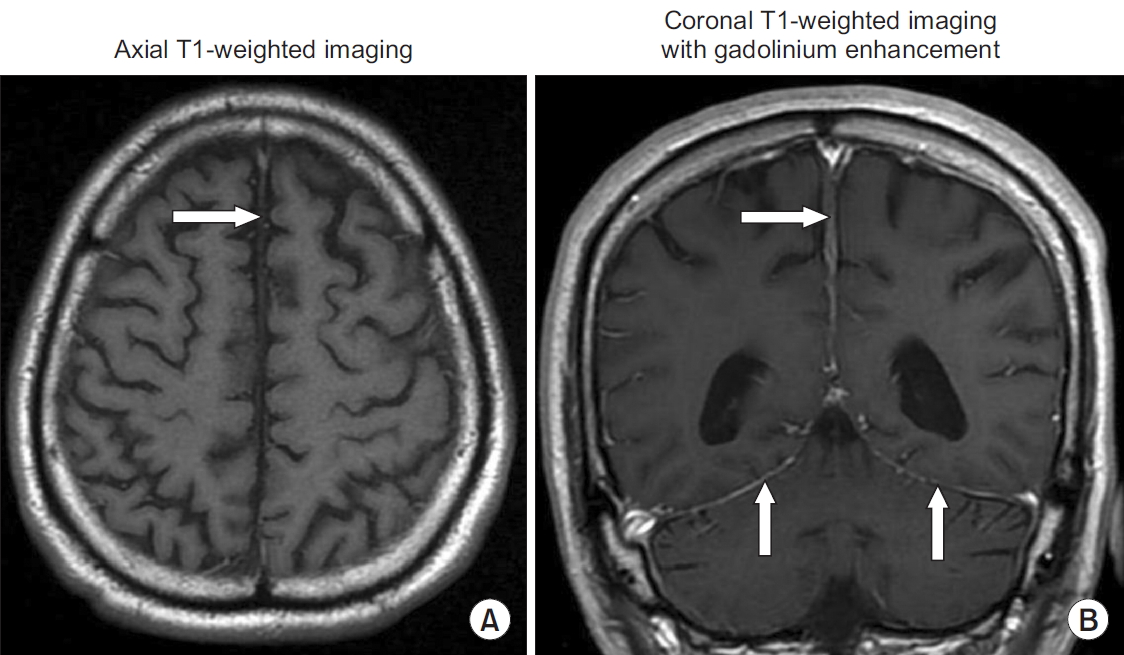
A 66-year-old man presented with fever and headache that had lasted for 3 months. The headache had a continuous pressing quality and bilateral involvement. He had a history of undifferentiated arthritis, for which he had undergone a treatment with chroloquine, leading to disease remission 2 years prior. He also had long term hypertension and diabetes. Current medications included enalapril, metformin, and chroloquine. He was febrile with body temperature of 38.5°C. Neither nuchal rigidity nor lymphadenopathy was detected. The findings of other general and neurological examinations were unremarkable. Magnetic resonance imaging (MRI) of the brain revealed thickening of the falx cerebri with diffuse pachymeningeal enhancement (Figure 1). A lumbar puncture revealed an opening pressure of 200 mm H2O. Cerebrospinal fluid (CSF) analysis showed a white blood cell count of 785 cells/mm3 with 62% lymphocytes and 38% neutrophils, a protein level of 72 mg/dL, and a glucose level of 80 mg/dL (concurrent a blood glucose level of 182 mg/dL). The results of Gram and Ziehl-Neelsen staining, India ink preparation, cryptococcal antigen, tuberculosis polymerase chain reaction, and culture for bacteria were negative. The CSF culture, which was subsequently reported, was also negative for Mycobacterium tuberculosis . The adenosine deaminase (ADA) level in CSF, which was determined by an automated method, was 11.1 U/L. Blood serological study for Venereal Disease Research Laboratory was nonreactive. The result of a chest X-ray was within the normal limits. The patient denied performing the meningeal biopsy. Diffuse hypertrophic pachymeningeal tuberculosis was suspected due to the patient having symptoms of prolonged fever and headache, lymphocytic CSF pleocytosis with elevated protein level and low CSF-to-serum glucose ratio, and a high level of CSF-ADA. The patient was treated with combined antituberculous drugs [isoniazid (I), rifampin (R), pyrazinamide (Z), ethambutol (E)], for 2 months, followed by IR (isoniazid, rifampin) for 4 months [1]. The fever and headache gradually disappeared. A follow-up MRI of the brain revealed a marked decreased in the thickening of the falx cerebri and pachymeningeal enhancement (Figure 2). The results of repeat CSF analysis and the level of CSF-ADA were within normal ranges.

Magnetic resonance imaging of a patient with diffuse hypertrophic pachymeningeal tuberculosis (before treatment). T1-weighted magnetic resonance imaging and with contrast enhancement showed thickened falx cerebri (arrow in A) with diffuse dural enhancement (arrows in B).
Magnetic resonance imaging of a patient with diffuse hypertrophic pachymeningeal tuberculosis (after treatment). T1-weighted magnetic resonance imaging and with contrast enhancement revealed a marked decrease in the thickening of the falx cerebri (arrow in A) and pachymeningeal enhancement (arrows in B), compared with Figure 1.
Hypertrophic pachymenigitis is a rare disease and consists of localized or diffuse thickening of the dura mater. It can involve the cranial or the spinal dura or both. Neurological manifestations include chronic headache, cranial nerve palsies, and progressive other neurological deficits arising due to compression of neural structures by the enlarged dura mater. The etiologies of this disorder divide into primary (idiopathic) and secondary causes; including infections (tuberculosis, fungal infection, cysticercosis, syphilis), systemic disorders, and malignancies [2]. Initial diagnosis depends on radiological findings which reveals focal or diffuse thickening of the dura. Dural tuberculosis is rare and usually presents with localized involvement of the pachymeninges [3]. In this patient, the diagnosis of pachymeningeal tuberculosis was confirmed by clinical response to antituberculous treatment [4].
This report also demonstrates the clinical utility of CSF-ADA as a one of diagnostic tests in the diagnosis of central nervous system tuberculosis [5].
Notes
Authors’ Contributions
Conceptualization: Chotmongkol V, Khamsai S. Methodology: Chotmongkol V, Khamsai S. Formal analysis: Chotmongkol V. Data curation: Chotmongkol V, Khamsai S. Software: Chotmongkol V, Khamsai S. Validation: Chotmongkol V, Khamsai S. Writing - original draft preparation: Chotmongkol V. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
No funding to declare.
