 |
 |
| Tuberc Respir Dis > Volume 77(2); 2014 > Article |
|
Abstract
Hyaluronic acid is widely used in medical procedures, particularly in cosmetic procedures administered by physicians or nonmedical personnel. The materials used for cosmetic procedures by physicians as well as illegally by non-medical personnel can cause nonthrombotic pulmonary embolism (NTPE). We report the case of a woman with acute respiratory failure, neurologic symptoms and petechiae after an illegal procedure of hyaluronic acid dermal filler performed by an unlicensed medical practitioner 3 days before symptom onset. Although a few cases of NTPE after injection of hyaluronic acid have been reported yet, this is the first typical case showing a NTPE manifestation after the facial injection of hyaluronic acid.
Hyaluronic acid is widely used in cosmetic procedures such as lip augmentation and the correction of facial wrinkles1,2. Here, we report the case of 35-year-old woman who developed dyspnea 3 days after an illegal hyaluronic acid dermal injection at a hair salon. She subsequently developed a confused mental state and petechial rash on the upper trunk, which is a typical clinical manifestation of nonthrombotic pulmonary embolism (NTPE). She was diagnosed with NTPE on the basis of her medical history and chest computed tomography (CT) results. She was fully recovered after conservative treatment. Although a few cases of NTPE after hyaluronic injection have been reported, the case with typical manifestation after facial area injection was rare.
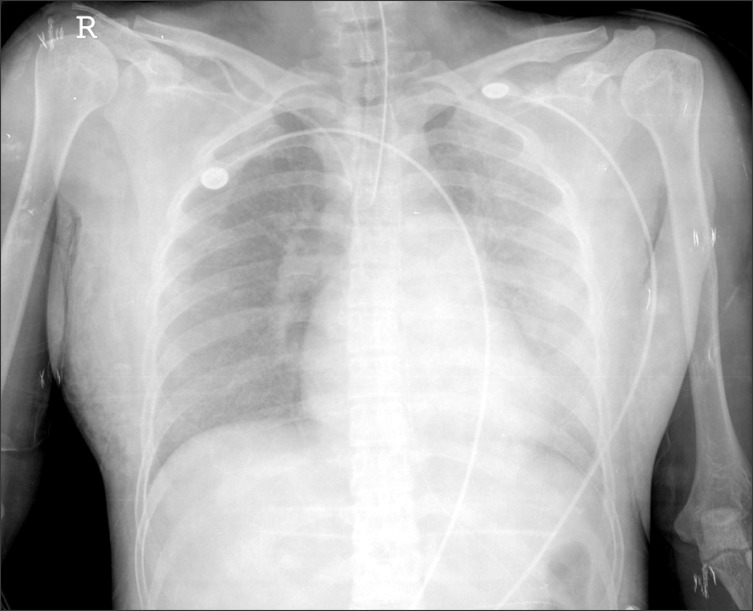
A 35-year-old woman who was previously healthy presented with abrupt onset of dyspnea and loss of consciousness for 5 minutes. Three days earlier, she received an illegal hyaluronic acid injection performed by an unlicensed medical practitioner into the dermis of the forehead and right cheek area. On physical examination, vital signs were as follows: body temperature, 36.8Ōäā; blood pressure, 150/110 mm Hg; pulse rate, 127/min; respiratory rate, 28/min. Mental status was confused. Crackles were revealed in both lower lung fields. Routine laboratory test including liver function test and renal function test showed normal range of results. And, complete blood count was as follows: white blood cells, 21,080/┬ĄL (neutrophils 91%); hemoglobin, 11 g/dL; platelets, 240,000/┬ĄL. Troponin I, 0.16 ng/mL (normal, 0-0.1 ng/mL); CK-MB, 0.6 ng/mL (normal, 0-3.6 ng/mL); C-reactive protein, 5.307 mg/dL (normal, 0-0.5 mg/dL); D-dimer, 1.278 ┬Ąg/mL (normal, 0-0.5 ┬Ąg/mL); and N-terminal of the prohormone brain natriuretic peptide was 9,177 pg/mL (normal, 0-124 pq/mL). Arterial blood gas analysis via 15 L O2 reservoir bag was as follows: pH, 7.505; PCO2, 28.6 mm Hg; PO2, 66.1 mm Hg; HCO3-, 22.4 mmol/L. Plain chest radiography showed ground glass opacity and consolidation in both lung fields (Figure 1). Contrast-enhanced chest CT showed diffuse ground glass opacity in both lungs with dilatation of the pulmonary artery and right ventricle (Figure 2).
The patient was admitted to the intensive care unit and treated with mechanical ventilation owing to worsening hypoxemia. After several days, hemorrhagic eruptions occurred in anterior chest area. She was initially administered antibiotics, corticosteroids and diuretics. Hypoxemia was gradually improved. After 5 days, the result of initial blood culture showed no growth and there was no evidence of fever. Therefore, we could exclude the septic embolism and discontinued the antibiotics. She was weaned from mechanical ventilation. At the eighth day of hospital admission, she was discharged. After one month, she was completely improved and follow-up chest CT showed improvement of the previous pulmonary lesion without fibrosis (Figure 3).
NTPE is defined as an embolization in the pulmonary circulation that can be caused by a variety of nonthrombotic embolic agents3. Different cell types (e.g., adipocytes, hematopoietic cells, amniotic cells, trophoblasts, and tumor cells), bacteria, fungi, foreign materials and gasses in the bloodstream may form an embolism in the pulmonary circulation4. NTPE can occur as a result of endothelial or parenchymal injury, causing inflammatory reactions in both systemic and pulmonary circulation3.
Hyaluronic acid is approved dermal filler used to correct facial wrinkles and folds2. Because the chemical structure of hyaluronic acid is conserved among all species, the potential for immunologic reactions and implant rejection is negligible. Thus, hyaluronic acid is a very suitable material for use as a dermal filler1. Common side effects of dermal injections of hyaluronic acid include acneiform eruptions, lumps, inflammatory nodules, blue bumps (i.e., the Tyndall effect), vascular occlusion and granulomas5. However, rare cases of NTPE were reported after injection of hyaluronic acid. Two cases were reported pulmonary embolism after an intra-articular injection of methylprednisolone and hyaluronate6,7. In that case, shortness of breath occurred after a knee injection of hyaluronic acid and multiple patchy ground glass opacities were observed bilaterally in the middle and lower lobes of the lungs on chest CT; biopsy revealed an amorphous material containing hyaluronic acid with fibrin. Park et al.2 report a case of NTPE syndrome after an illegal hyaluronic acid vaginal injection3. Progressive dyspnea and decreased consciousness were observed 3 days after the injection; chest CT revealed bilateral ground glass opacity from the lower to apical zone, and biopsy confirmed a granulomatous foreign body reaction as observed in talc embolism2.
This case was exhibited progressive dyspnea 3 days after hyaluronic acid dermal injection with hypoxemia, petechiae on the anterior chest wall and bilateral ground glass opacity on chest CT. In addition, chest CT showed basal dominant diffuse ground glass opacity, pulmonary artery dilatation, and cardiomegaly on the right side. Finding of this chest CT was distinguished from the finding of septic embolism which include multiple peripheral nodule, wedge-shaped peripheral leision, cavitation of nodules, and a feeding vessel sign8. Also, the ground glass opacity distribution did not correspond to idiopathic interstitial pneumonia.
In the case reported by Park et al.2 NTPE was believed to have occurred in the systemic circulation, because hyaluronic acid was injected to the anterior wall of vagina where extensive venous plexus exists. In addition, Bhagat et al.7 suggest NTPE occurs as a result of hyaluronic acid embolisms in the systemic circulation due to damage to the synovium as a result of hyaluronic acid injection. Analyzing the results of cases of various illegal silicone injections shows pulmonary silicone embolism can occur via several mechanisms such excessive local tissue pressure induced by large-dose and high-pressure injection, local massage by an unlicensed practitioner, migration effect, or direct intravascular injections9. As review of the above mentioned cases suggests the NTPE in the present patient occurred as a result of damage to facial soft tissues due to inappropriate anatomical location and injection by an unlicensed practitioner as well as the inflow of hyaluronic acid embolisms directly into the blood vessels. Although hyaluronic acid binds to endothelial cells throughout the body, it binds particularly well to the pulmonary vasculature10. The symptoms in the present case were due to mechanical obstruction caused by hyaluronic acid bound to the endothelial cells of the pulmonary vasculature. Accordingly, CT showed dilatation of the pulmonary artery and right ventricular enlargement. NTPE was diagnosed on the basis of clinical conditions and chest CT. Severe hypoxia improved after conservative treatment with mechanical ventilation, which led to rapid recovery. Follow-up chest CT revealed improvements without fibrosis, confirming the diagnosis of NTPE rather than other possibilities as a result of interstitial lung disease.
Although cases of NTPE caused by hyaluronic acid injection are occasionally reported, this is the first typical case shown to NTPE manifestation after facial injection of hyaluronic acid.
References
1. Matarasso SL, Carruthers JD, Jewell ML. Restylane Consensus Group. Consensus recommendations for soft-tissue augmentation with nonanimal stabilized hyaluronic acid (Restylane). Plast Reconstr Surg 2006;117(3 Suppl):3S-34S. PMID: 16531934.


2. Park HJ, Jung KH, Kim SY, Lee JH, Jeong JY, Kim JH. Hyaluronic acid pulmonary embolism: a critical consequence of an illegal cosmetic vaginal procedure. Thorax 2010;65:360-361. PMID: 20388764.


3. Bach AG, Restrepo CS, Abbas J, Villanueva A, Lorenzo Dus MJ, Schopf R, et al. Imaging of nonthrombotic pulmonary embolism: biological materials, nonbiological materials, and foreign bodies. Eur J Radiol 2013;82:e120-e141. PMID: 23102488.


4. Jorens PG, Van Marck E, Snoeckx A, Parizel PM. Nonthrombotic pulmonary embolism. Eur Respir J 2009;34:452-474. PMID: 19648522.


5. Schanz S, Schippert W, Ulmer A, Rassner G, Fierlbeck G. Arterial embolization caused by injection of hyaluronic acid (Restylane). Br J Dermatol 2002;146:928-929. PMID: 12000405.


6. Famularo G, Liberati C, Sebastiani GD, Polchi S. Pulmonary embolism after intra-articular injection of methylprednisolone and hyaluronate. Clin Exp Rheumatol 2001;19:355PMID: 11407098.

7. Bhagat R, Forteza RM, Calcote CB, Williams WT, Bigler SA, Dwyer TM. Pulmonary emboli from therapeutic sodium hyaluronate. Respir Care 2012;57:1670-1673. PMID: 22417476.


8. Kuhlman JE, Fishman EK, Teigen C. Pulmonary septic emboli: diagnosis with CT. Radiology 1990;174:211-213. PMID: 2294550.


9. Price EA, Schueler H, Perper JA. Massive systemic silicone embolism: a case report and review of literature. Am J Forensic Med Pathol 2006;27:97-102. PMID: 16738424.


10. Szczepanek K, Kieda C, Cichy J. Differential binding of hyaluronan on the surface of tissue-specific endothelial cell lines. Acta Biochim Pol 2008;55:35-42. PMID: 18231653.





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




