 |
 |
| Tuberc Respir Dis > Volume 78(3); 2015 > Article |
|
Abstract
Background
Although organizing pneumonia (OP) responds well to corticosteroid therapy, relapse is common during dose reduction or follow-up. Predictors of relapse in OP patients remain to be established. The aim of the present study was to identify factors related to relapse in OP patients.
Methods
This study was retrospectively performed in a tertiary referral center. Of 66 OP patients who were improved with or without treatment, 20 (30%) experienced relapse. The clinical and radiologic parameters in the relapse patient group (n=20) were compared to that in the non-relapse group (n=46).
Results
Multivariate analysis demonstrated that percent predicted forced vital capacity (FVC), PaO2/FiO2, and serum protein level were significant predictors of relapse in OP patients (odds ratio [OR], 0.82; 95% confidence interval [CI], 0.70-0.97; p=0.018; OR, 1.02; 95% CI, 1.00-1.04; p=0.042; and OR, 0.06; 95% CI, 0.01-0.87; p=0.039, respectively).
Organizing pneumonia (OP) is a distinct type of interstitial lung disease (ILD), that is, pathologically characterized by organization within alveolar ducts and alveoli ("organizing pneumonia") with or without organization within bronchioles ("polypoid bronchiolitis obliterans")1, although OP can be a focal process2. In its primary form, OP is known as cryptogenic organizing pneumonia (COP) whereas the secondary form is associated with various conditions or causes, such as collagen-vascular diseases, hematologic disorders, drugs, inflammatory bowel disease, and radiotherapy1,2,3,4.
Regardless cryptogenic or secondary OP, the majority of OP patients achieve a good prognosis; the response rate is 65-85% on corticosteroid therapy1. However, relapse rates of OP range from 13% to 58%, after corticosteroids are decreased or discontinued2,3,5,6,7. Previous reports have suggested delayed treatment5, hypoxemia6, and multifocal opacity on chest radiograph7 as predictors related to relapse in OP, but these results were not reproduced by subsequent studies. Thus, the predictors of relapse in OP patients remain to be established.
The aim of the present study was to elucidate factors related to relapse in OP patients. To achieve this, patients were allocated to a relapse or non-relapse group and these two groups were compared with respect to clinical and radiologic parameters.
The medical records of patients hospitalized and diagnosed with OP at Kyungpook National University Hospital (KNUH), a tertiary referral center, in Daegu, South Korea between March 2002 and December 2012 were retrospectively reviewed. OP was diagnosed by multidisciplinary discussion of clinician, radiologists, and pathologists. The pathologic pattern of OP was defined as patchy airspace organization with fibroblastic tissue within alveoli and alveolar ducts with or without bronchiolar involvement and variable interstitial changes, such as type 2 alveolar epithelial cell proliferation and interstitial chronic inflammatory infiltrates2. Pathologic specimens were obtained by surgical lung biopsy, transbronchial lung biopsy, or percutaneous needle biopsy. Patients diagnosed based on a non-surgical biopsy specimen required typical computed tomographic (CT) findings of OP, which included patchy consolidation or ground glass opacity (GGO) with a peribronchial or subpleural distribution without extensive reticulation or honeycombing4. The exclusion criteria applied were as follows: (1) focal OP2 (only ILD form was included) and (2) cases which responded to antibiotic therapy. As described in a previous study5, relapse was defined as the appearance of characteristic new infiltrates by chest radiography with compatible clinical symptoms after corticosteroid administration was stopped or the dose was reduced. This study was approved by the Institutional Review Board of the KNUH, which waived the requirement for written informed consent because of the retrospective nature of the study.
Demographic data including age, gender, and body mass index, and smoking history at presentation were checked, and comorbid conditions and duration of corticosteroid therapy were reviewed. Blood laboratory findings, including leukocyte count, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), protein, albumin, liver function test, procalcitonin, N-terminal-pro-B-type natriuretic peptide (NT-proBNP), lactate dehydrogenase (LDH), were included in the check list. Bronchoalveolar lavage (BAL) fluid analysis included total and differential cell counts and lymphocyte subset data. Arterial blood gas analysis data, such as partial pressure of oxygen (PaO2) and carbon dioxide (PaCO2) in arterial blood, and PaO2/fraction of inspired oxygen (FiO2) and lung function data, such as percent predicted forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCO), were reviewed.
Chest CT findings were reviewed by two chest radiologists (K.-M.S. and J.-K.L.) unaware of clinical information. When the readings of the two radiologists were discrepant, a final decision was reached by consensus. The presences of consolidation, GGO, and reticulation were checked, and the extents of these lesions were estimated at three levels, resulting in a total six lung zones8. Average extents of GGO, consolidation, and reticulation were scored to the nearest 5% in each zone, as previously described9. The upper zone was defined as at or above the aortic arch, the middle zone was defined as between the aortic arch and pulmonary veins, and the lower zone was defined as at or below the pulmonary veins9.
Statistical analysis was performed using SPSS version 20.0 (IBM Co., Armonk, NY, USA). Data are expressed as means with standard deviations or medians with interquartile ranges (IQR) for continuous variables and numbers with percentages for categorical variables. The Student's t test or Mann-Whitney U test was used to compare continuous variables between relapse and non-relapse groups, and the chi-squared test or Fisher exact test was used to compare categorical variables. Multivariable logistic regression analysis was used to identify predictors of relapse in OP patients. The Hosmer-Lemeshow test was used as a test to assess the goodness-of-fit of logistic regression models. p-values of <0.05 were considered to indicate statistical significance.
Seventy-three patients with OP were identified. Mean patient age was 57┬▒11 years with female preponderance (n=45, 62%). Never-smokers (n=50, 68%) were more common than ever-smokers. Pathologic OP patterns were identified by surgical lung biopsy in 42 patients (58%), transbronchial lung biopsy in 22 (30%), or percutaneous needle biopsy in 9 (12%). Secondary OP (n=24, 33%) was associated with collagen-vascular disease (n=8; rheumatoid arthritis, n=4; systemic lupus erythematosus, n=2; and polymyositis, n=2), radiation therapy (n=7), drugs (n=6), hematopoietic stem cell transplantation (n=1), ulcerative colitis (n=1), and mycoplasma pneumonia (n=1).
With the exception of one patient with polythiouracil-induced OP, all patients received corticosteroid treatment with or without immunosuppressant including azathioprine (n=1) and cyclosporine (n=1). Response to therapy could not be assessed in three patients due to follow-up loss (n=2) or no available medical record (n=1). Of the 70 remaining patients, 66 (94%) improved with or without treatment, and of these, 20 (30%) experienced relapse. The other four patients died from disease progression (n=3) or pneumonia (n=1). Median follow-up duration was 19 months (IQR, 7-48 months), median duration of corticosteroid administration before relapse was 6 months (IQR, 4-12 months), and median time from corticosteroid discontinuation to relapse was 2 months (IQR, 0.2-6 months).
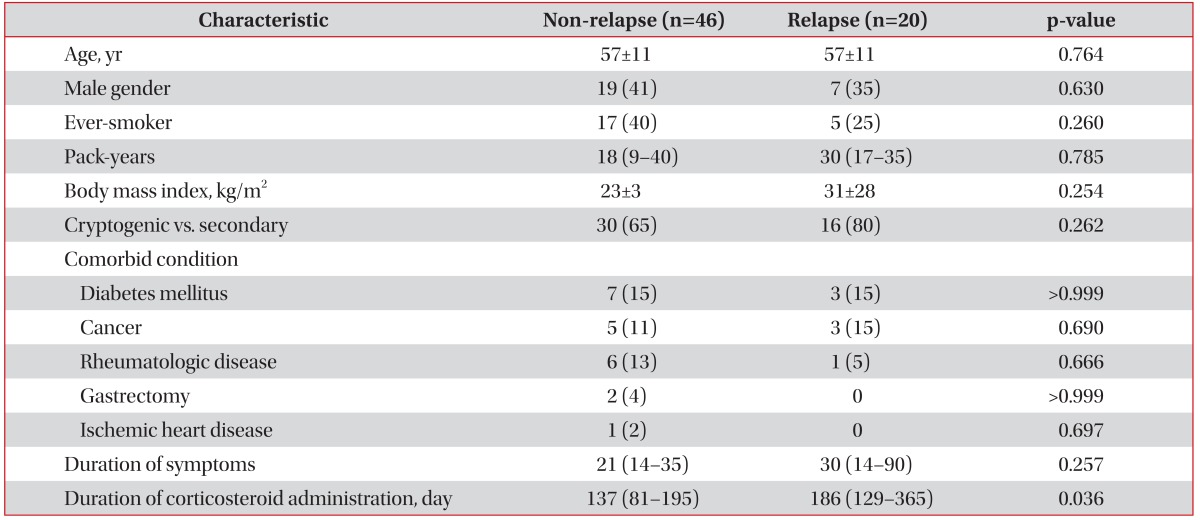
Baseline and clinical characteristics are presented in Table 1. Age, gender, body mass index, smoking history, comorbid conditions, and the prevalence of secondary OP were not significantly different in the relapse and non-relapse groups. However, the duration of corticosteroid treatment before relapse was significantly longer in the relapse group, as compared with the total duration of corticosteroid therapy in the non-relapse group (186 days [129-365 days] vs. 137 days [81-195 days], p=0.036). When patients were classified by the duration of corticosteroid administration (within 3 months, 4-6 months, 7-9 months, and more than 9 months), the relapse rate during each time interval was 19%, 29%, 25%, and 58%.
ESR, CRP, procalcitonin, NT-proBNP, and LDH levels were not significantly different between the two groups (Table 2). However, mean serum protein level was significantly lower and mean serum albumin level tended to be lower in the relapse group (6.8┬▒0.67 g/dL vs. 4┬▒0.8 g/dL, p=0.003; and 3.5 g/dL [3.2-3.8 g/dL] vs. 3.7 g/dL [3.5-4.0 g/dL], p=0.070). No significant intergroup difference was found in other parameters of liver function test. PaO2/FiO2 tended to be higher in the relapse group (396┬▒85 mm Hg vs. 356┬▒71 mm Hg, p=0.077), but no significant differences were observed for PaO2 and PaCO2.
Of BAL fluid analysis data, total and differential cell counts and lymphocyte subsets showed no significant differences. However, the relapse group had significantly lower percentage of FVC predicted value and tended to have a higher percentage of predicted DLCO value than the non-relapse group (70┬▒15% pred. vs. 86┬▒21% pred., p=0.009; and 62┬▒25% pred. vs. 77┬▒27% pred., p=0.057, respectively).
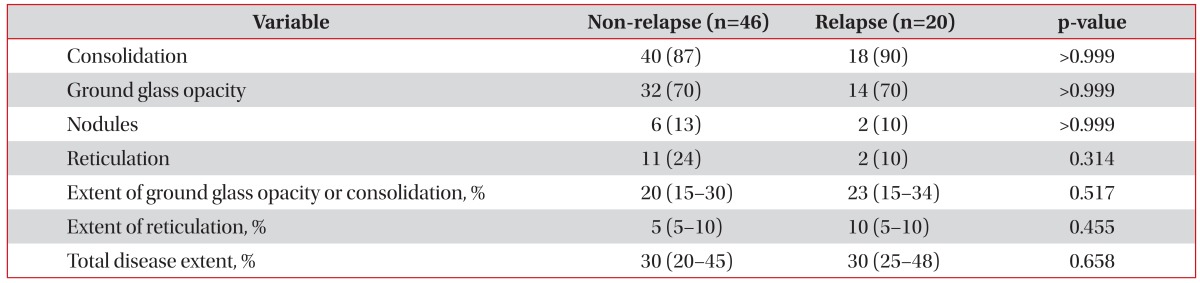
Between the two groups, no significant differences in CT findings were found, and extents of GGO or consolidation and reticulation and total disease extent were not significantly different (Table 3).
Multivariate logistic regression analysis was used to identify predictors of relapse (Table 4). Age, female gender, and variables with p-values of <0.1 by univariate analysis were subjected to multivariate analysis. However, serum albumin was excluded because of its significant correlation with serum protein. Percent predicted FVC, PaO2/FiO2, and serum protein level were found to be independent predictors of relapse in OP patients (odds ratio [OR], 0.82; 95% confidence interval [CI], 0.70-0.97, p=0.018; OR, 1.02; 95% CI, 1.00-1.04; p=0.042; and OR, 0.06; 95% CI, 0.01-0.87; p=0.039, respectively). The Hosmer-Lemeshow test indicated that the overall model fit was good (p=0.883).
The present study shows FVC, PaO2/FiO2, and serum protein level significantly predict relapse in OP. In fact, FVC and PaO2/FiO2 are known to reflect disease severity at presentation, which suggests patients with severe OP are more likely to relapse.
Delayed treatment5, hypoxemia6, multifocal opacity by chest radiography7, and a shorter maintenance of initial steroid dose7 have been previously suggested to be predictors of OP relapse. Of these predictors, hypoxemia and multifocal opacity are known to be associated with disease severity at presentation. In the present study, FVC and PaO2/FiO2 were found to independently predict OP relapse, which encourage us to speculate that reduction in FVC is associated with disease extent. However, no significant differences were observed between the relapse and non-relapse groups with respect to area of GGO or consolidation, reticulation, or overall disease by CT scan. We are unable to explain the observed discrepancy between physiologic and morphologic parameters with respect to disease extent. Furthermore, we found PaO2/FiO2, as a parameter of hypoxia, significantly predicted relapse, which concurs with a previous findings regarding hypoxemia as a predictor of relapse in OP6. This finding also suggests that the severity of OP at presentation is related to subsequent relapse. In the present study, the duration of corticosteroid administration was determined by each physician's judgement, not predefined protocol. Consequently, corticosteroids were administered for a longer period of time in the relapse group than in the non-relapse group in contrast of the previous study7. Furthermore, when patients were divided by the duration of corticosteroid administration, the relapse rate was higher in the subgroup of >9 months.
In the present study, a lower serum protein level independently predicted relapse. This finding cannot be fully explained. In a previous study, connective tissue disease-associated OP tended to have a higher recurrence rate than COP4, and in another study6, the serum protein and albumin levels were significantly lower in patients that relapsed. Based on these findings, we speculate that low serum protein levels are derived from associated or underlying diseases. However, in the present study, secondary OP and comorbid condition prevalence did not differ significantly in the relapse and non-relapse groups. This is in accordance with the finding of the previous studies that there was no difference in the relapse rate between secondary OP and COP7,10. Therefore, the possibility that low serum protein level was caused by the severity of OP itself should be considered. This assumption supports the concept that the severity of OP at presentation is related to subsequent relapse.
The present study has several limitations. First, since the study was performed retrospectively, selection bias could not be avoided. Second, not all patients underwent surgical lung biopsy, and thus, in these patients, diagnoses were not confirmatory. However, typical CT findings of OP were required, thereby minimizing the misdiagnosis of OP. Thirdly, the number of subjects enrolled was too small to allow us to conclude that the identified parameters are independent predictors of OP relapse. Furthermore, given the fact that in the present study, subjects were collected for more than 10 years, and in previous studies4,5,6,7, sample sizes were all small, a large-scale multicenter study is required to confirm our findings.
In conclusion, parameters related to disease severity, such as FVC and PaO2/FiO2 and serum protein at presentation are significant predictors of relapse in OP patients.
References
1. Demedts M, Costabel U. ATS/ERS international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Eur Respir J 2002;19:794-796. PMID: 12030715.


2. Lohr RH, Boland BJ, Douglas WW, Dockrell DH, Colby TV, Swensen SJ, et al. Organizing pneumonia: features and prognosis of cryptogenic, secondary, and focal variants. Arch Intern Med 1997;157:1323-1329. PMID: 9201006.


3. Drakopanagiotakis F, Paschalaki K, Abu-Hijleh M, Aswad B, Karagianidis N, Kastanakis E, et al. Cryptogenic and secondary organizing pneumonia: clinical presentation, radiographic findings, treatment response, and prognosis. Chest 2011;139:893-900. PMID: 20724743.


4. Yoo JW, Song JW, Jang SJ, Lee CK, Kim MY, Lee HK, et al. Comparison between cryptogenic organizing pneumonia and connective tissue disease-related organizing pneumonia. Rheumatology (Oxford) 2011;50:932-938. PMID: 21169342.



5. Lazor R, Vandevenne A, Pelletier A, Leclerc P, Court-Fortune I, Cordier JF. Cryptogenic organizing pneumonia. Characteristics of relapses in a series of 48 patients. The Groupe d'Etudes et de Recherche sur les Maladles "Orphelines" Pulmonaires (GERM"O"P). Am J Respir Crit Care Med 2000;162:571-577. PMID: 10934089.


6. Watanabe K, Senju S, Wen FQ, Shirakusa T, Maeda F, Yoshida M. Factors related to the relapse of bronchiolitis obliterans organizing pneumonia. Chest 1998;114:1599-1606. PMID: 9872195.


7. Barroso E, Hernandez L, Gil J, Garcia R, Aranda I, Romero S. Idiopathic organizing pneumonia: a relapsing disease. 19 years of experience in a hospital setting. Respiration 2007;74:624-631. PMID: 17536184.


8. Lee JS, Lynch DA, Sharma S, Brown KK, Muller NL. Organizing pneumonia: prognostic implication of high-resolution computed tomography features. J Comput Assist Tomogr 2003;27:260-265. PMID: 12703023.


9. Best AC, Meng J, Lynch AM, Bozic CM, Miller D, Grunwald GK, et al. Idiopathic pulmonary fibrosis: physiologic tests, quantitative CT indexes, and CT visual scores as predictors of mortality. Radiology 2008;246:935-940. PMID: 18235106.


10. Sveinsson OA, Isaksson HJ, Sigvaldason A, Yngvason F, Aspelund T, Gudmundsson G. Clinical features in secondary and cryptogenic organising pneumonia. Int J Tuberc Lung Dis 2007;11:689-694. PMID: 17519103.

Table┬Ā2
Laboratory data
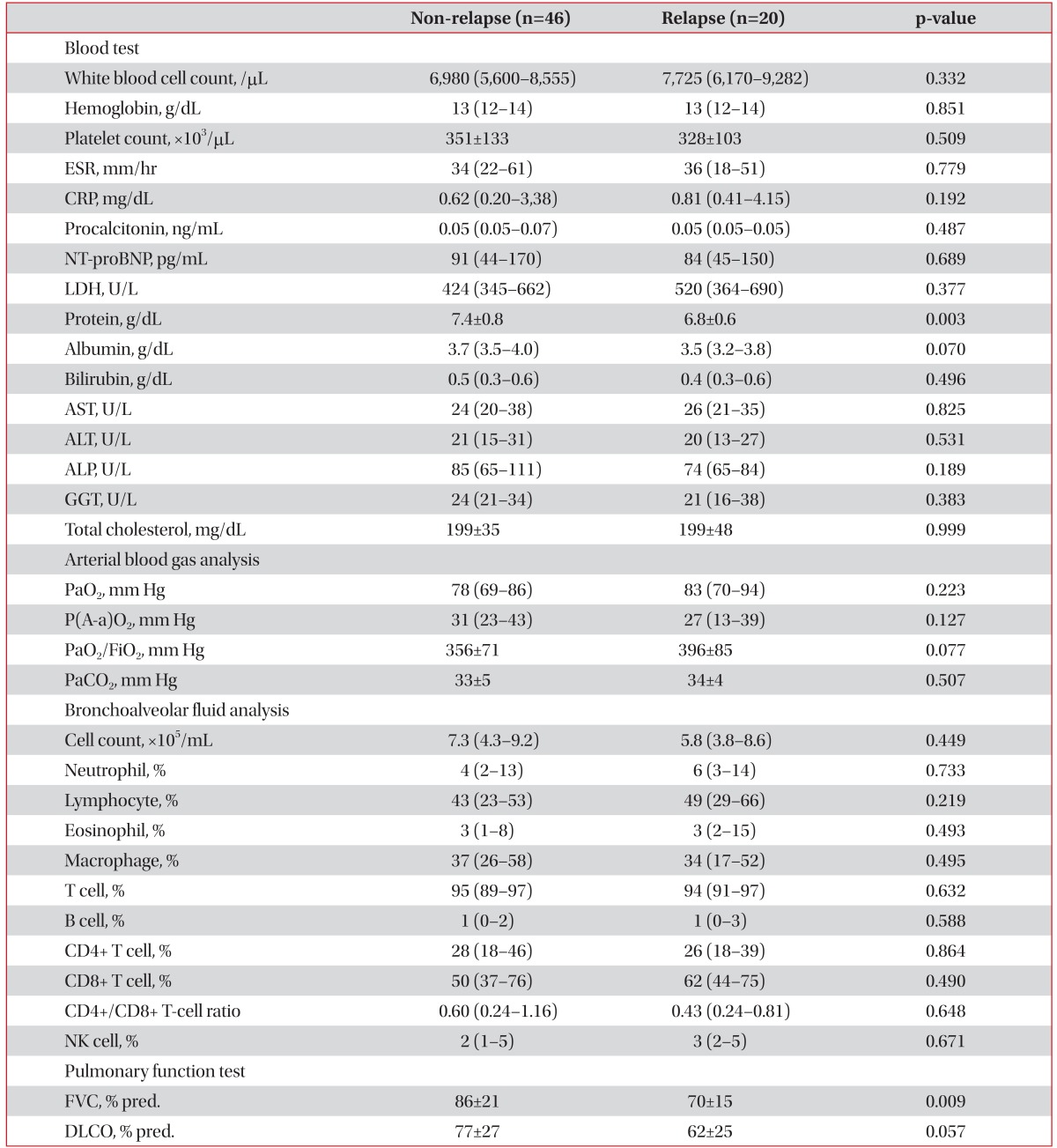
ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; NT-proBNP: N-terminal-pro-B-type natriuretic peptide; LDH: lactate dehydrogenase; AST: aspartate transaminase; ALT: alanine transaminase; ALP: alkaline phosphatase; GGT: gamma-glutamyl transferase; PaO2: partial pressure of oxygen in arterial blood; P(A-a)O2: alveolar-arterial partial oxygen gradient; PaO2/FiO2: PaO2/fraction of inspired oxygen; PaCO2: partial pressure of carbon dioxide in arterial blood; NK: natural killer; FVC: forced vital capacity; DLCO: diffusing capacity for carbon monoxide.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




