 |
 |
| Tuberc Respir Dis > Volume 82(4); 2019 > Article |
|
Abstract
Background
Although the frequency of respiratory viral infection in patients with pulmonary acute respiratory distress syndrome (ARDS) is not uncommon, clinical significance of the condition remains to be further elucidated. The purpose of this study was to compare characteristics and outcomes of patients with pulmonary ARDS infected with influenza and other respiratory viruses.
Methods
Clinical data of patients with pulmonary ARDS infected with respiratory viruses January 2014-June 2018 were reviewed. Respiratory viral infection was identified by multiplex reverse transcription-polymerase chain reaction (RT-PCR).
Results
Among 126 patients who underwent multiplex RT-PCR, respiratory viral infection was identified in 46% (58/126): 28 patients with influenza and 30 patients with other respiratory viruses. There was no significant difference in baseline and clinical characteristics between patients with influenza and those with other respiratory viruses. The use of extracorporeal membrane oxygenation (ECMO) was more frequent in patients with influenza than in those with other respiratory viruses (32.1% vs 3.3%, p=0.006). Co-bacterial pathogens were more frequently isolated from respiratory samples of patients with pulmonary ARDS infected with influenza virus than those with other respiratory viruses. (53.6% vs 26.7%, p=0.036). There were no significant differences regarding clinical outcomes. In multivariate analysis, acute physiology and chronic health evaluation II was associated with 30-mortality (odds ratio, 1.158; 95% confidence interval, 1.022-1.312; p=0.022).
Acute respiratory distress syndrome (ARDS) is one of the chief conditions for which patients are admitted to the intensive care unit (ICU) and contributes to substantial mortality rates1. Respiratory viral infection is not uncommon in critically ill patients who received invasive mechanical ventilation due to respiratory failure2. Some studies have reported that the frequency of respiratory viral infection ranged from 13.4% to 49%3,4,5. Availability of multiplex reverse transcription-polymerase chain reaction (RT-PCR) has facilitated the identification of respiratory viral infection6. Among the diverse risk factors for ARDS, respiratory viral infection has been shown to contribute to development and progression of pulmonary ARDS7,8. Although several studies have reported the clinical impact of respiratory viruses on critically ill patients3,9, further studies are needed to clarify the significance on those with pulmonary ARDS. Influenza viral infection in pulmonary ARDS has gained attention to intensivists due to high morbidity and mortality10,11, but little data comparing characteristics and outcomes of the different types of viruses in patients with pulmonary ARDS. Moreover, differences in clinical outcomes between patients infected with influenza and other respiratory viruses have not been clearly elucidated.
The aim of this study was to compare the characteristics and clinical outcomes of patients with pulmonary ARDS infected with influenza vs. other respiratory viruses.
Patients diagnosed with pulmonary ARDS who were admitted to the medical ICU at a tertiary hospital and received invasive mechanical ventilation were searched from January 2014 to June 2018. ARDS was fulfilled for the Berlin diagnostic criteria12. Among them, those who underwent RT-PCR for respiratory viral infection were reviewed. Respiratory specimens such as bronchial and endotracheal aspirate, nasopharyngeal swab or sputum were obtained for RT-PCR analysis. AdvanSure RV real-time RT-PCR (LG Chemistry, Seoul, Korea) assay based on the multiplex polymerase chain reaction method was used to identify respiratory viruses (influenza virus, parainfluenza virus, respiratory syncytial virus, adenovirus, metapneumovirus, rhinovirus, bocavrius, and coronavirus). Baseline (age, sex, body mass index, and comorbidities) and clinical characteristics (Acute Physiology and Chronic Health Evaluation [APACHE] II score, Sequential Organ Failure Assessment [SOFA] score, clinical complications [shock, acute kidney injury], management, etc.) were assessed. Additionally, data from laboratory (neutrophil count, lymphocyte count, hemoglobin, platelet, C-reactive protein [CRP] level, total protein level, albumin level, etc.), microbiologic data (types of respiratory virus, co-respiratory bacterial or fungal pathogens) and clinical outcomes (length of stay in ICU and hospital, mortality) were analyzed. This study was approved by the Institutional Review Board of Gyeongsang National University Hospital (No. 2018-05-015). Informed consent was waived due to retrospective nature of the study. The study was in accordance with the ethical standards of institutional and/or national research committees and with the Helsinki declaration and its later amendments or comparable ethical standards.
Continuous data were expressed as mean±standard deviation (SD) and compared using the Mann-Whitney U test. Non-continuous data were expressed as numbers and percentages and were analyzed using the chi-square or Fisher exact test. To evaluated factors associated with a 30-mortality, logistic regression analysis was used. Factors with p-value <0.1 in univariate analysis were entered into multivariate analysis. All data were analyzed using the SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA).
One hundred sixty-seven patients with pulmonary ARDS were admitted to the medical ICU. Figure 1 shows flow of patients with ARDS during the period. One hundred and twenty-six patients with pulmonary ARDS (75.4%) underwent multiplex RT-PCR to evaluate the presence of respiratory viral infection, which was identified in 46% (58/126) subjects. Community-acquired respiratory viral infection was identified in 37 of 85 patients (43.5%) with community-acquired ARDS whereas hospital-acquired respiratory infection was detected in 21 of 41 those with hospital-acquired ARDS (51.2%) (p=0.417).
The mean age of patients was 67.6±13.3 years and the proportion of men was 70.7%. In all cases, the risk factor for pulmonary ARDS was pneumonia. Twenty-eight patients (48.3%) were infected with influenza virus while other respiratory viruses were identified in 30 patients (51.7%). Table 1 shows the characteristics of patients with influenza and those with other respiratory virus infection. There was no significant difference regarding baseline characteristics, severity of illness and clinical complications between patients with influenza and those with other respiratory viruses. Extracorporeal membrane oxygenation (ECMO) was significantly more used in patients with influenza virus than those with other respiratory viruses as a rescue therapy (32.1% vs. 3.3%, p=0.006).
Table 2 compares laboratory results and radiologic scores of patients with influenza and those with other viruses. There was a trend toward higher hemoglobin and CRP levels in patients with influenza than in those with other respiratory viruses. No significant difference was observed in other parameters between the two groups. Transthoracic echocardiography was done in 75.9% (44/58) patients on admission of medical intensive care unit to evaluate acute heart failure. The mean ejection fraction was 59.2%±7.76%. Stress induced cardiomyopathy and right ventricular dysfunction were featured in three (6.7%) and five (11.1%) patients, respectively.
Table 3 enlists the types of respiratory viruses and corespiratory pathogens in patients with pulmonary ARDS. Influenza A was the most common virus (21 cases) and other respiratory virus infection (10 coronavirus, 5 RSV, 4 parainfluenza virus, 4 rhinovirus, 3 adenovirus, 3 metapneumovirus, and 1 bocavirus) were isolated. Overall 43.1% co-respiratory pathogens were isolated simultaneously. Patients with influenza presented with significantly higher co-bacterial pathogens than those with other respiratory viruses. Gram-positive bacteria co-infection was common in patients with influenza virus than those with other respiratory viruses (39.3% vs. 10%).
Clinical outcomes are presented and compared in Table 4. Patients with influenza virus were treated with neuraminidase inhibitor such as oseltamivir or peramivir but those any antiviral agent was not administered in those with other respiratory viruses. Overall ICU mortality and hospital mortality rates were 51.7% and 55.2%, respectively. There were no significant differences in extubation success, duration of mechanical ventilation, mortality, and length of stay in the ICU and hospital.
Multivariate analysis associated with 30-day mortality was performed and has been shown in Table 5. APACHE II score at admission was associated with ICU mortality. Influenza virus and co-bacterial infection were not associated with ICU mortality.
Factors associated with 30-day mortality are shown in Table 5. In univariate analysis, APACHE II, SOFA and low partial pressure of oxygen/fractioned inspired oxygen ratio were associated with 30-day mortality. APACHE II only was associated with a 30-day mortality in multivariate analysis. Fourteen patients were treated with steroid. The reasons of use of steroid were treatment of concomitant exacerbation of airway disease (n=4, 6.9%), refractory septic shock (n=4, 6.9%), and adjunct treatment of ARDS (n=6, 10.3%), which might not affect mortality in ARDS patients with respiratory viral infection.
The present study showed that approximately 46% patients with pulmonary ARDS had a concomitant respiratory viral infection and influenza A virus was most commonly isolated. Co-respiratory infection was more frequent in patients with influenza infection than in those with other respiratory viral infection. Although patients with influenza virus received more invasive treatment such as ECMO, clinical outcomes did not differ between patients with influenza infection and those with other viral infection. APACHE II was associated with ICU mortality in patients with pulmonary ARDS.
ARDS is a common reason of admission to the ICU in critically ill patients with one-quarter of the total number of patients receiving mechanical ventilation being diagnosed with the condition1. ARDS also contributes to substantial mortality in the ICU1. Various risk factors are associated with ARDS and pulmonary ARDS is frequently encountered in ICU. Pneumonia has been known as the most common etiology of pulmonary ARDS13. The co-infection of respiratory virus was found in patients with severe pneumonia admitted to ICU ranging from 13.4% to 49%3,4,5. The frequency of respiratory viral infection in pulmonary ARDS has not been established. The current study showed similar frequency of respiratory viral infection in pulmonary ARDS as those of severe pneumonia in patients admitted to the ICU. Respiratory viruses play a role in development and progression of ARDS8; therefore, it is important to elucidate the clinical significance of them in patients with pulmonary ARDS. Several studies have reported clinical outcomes in patients infected with respiratory viruses receiving mechanical ventilation14,15,16,17. In the present study, clinical outcomes did not differ between patients with infected with influenza virus and those with other respiratory viruses. Similar clinical outcomes were reported in patients with respiratory syncytial virus or rhinovirus compared to influenza virus17,18. In the current study, comparison of clinical outcomes in each respiratory viruses was not performed due to a few cases except for influenza virus. APACHE II score was associated with a 30-day mortality in patients with ARDS infected with respiratory viruses, which suggests that severity of illness has an impact on overall clinical outcomes.
In the present study, ECMO was more frequently used in patients with influenza virus than those with other respiratory virus. Several studies have reported the use of ECMO in case of refractory hypoxemia in patients with influenza-related ARDS14,19,20. However, the clinical implication of more frequent application of ECMO in patients with influenza virus should be interpreted cautiously in the present study. The use of ECMO is generally determined by multiple factors including the severity of illness, comorbidities of patients rather than types of respiratory viruses21.
In the current study, co-respiratory bacterial pathogens was in more than half of patients with influenza. The current study is consistent with previous studies that influenza virus infection was commonly complicated with co-infection by bacteria such as Staphylococcus aureus and Streptococcus pneumoniae22,23. This supports the use of empirical antibiotics in cases of ARDS infected with influenza virus.
The present study has several limitations. First, this study was conducted at a single center and analyzed data retrospectively, therefore selection bias cannot be excluded. Second, the site obtaining respiratory sample was not the same, therefore, whether respiratory viruses were pathogens cannot be accurately distinguished. The miss to detect respiratory viruses by multiplex RT-PCR cannot be ruled out. Third, the change in clinical decision by identifying respiratory viruses was not evaluated as in a previous study5. Fourth, the prone position was performed in the low proportion of patients with ARDS compared to a recent study1.
In conclusion, respiratory viral infection was frequently observed in patients with pulmonary ARDS as demonstrated by multiplex RT-PCR. Patients with influenza virus had more cobacterial infection and received ECMO than those with other respiratory viruses without significant difference with respect to clinical outcomes.
References
1. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016;315:788-800. PMID: 26903337.


2. Nguyen C, Kaku S, Tutera D, Kuschner WG, Barr J. Viral respiratory infections of adults in the intensive care unit. J Intensive Care Med 2016;31:427-441. PMID: 25990273.


3. Choi SH, Hong SB, Ko GB, Lee Y, Park HJ, Park SY, et al. Viral infection in patients with severe pneumonia requiring intensive care unit admission. Am J Respir Crit Care Med 2012;186:325-332. PMID: 22700859.


4. Karhu J, Ala-Kokko TI, Vuorinen T, Ohtonen P, Syrjala H. Lower respiratory tract virus findings in mechanically ventilated patients with severe community-acquired pneumonia. Clin Infect Dis 2014;59:62-70. PMID: 24729498.




5. Kim HJ, Choi SM, Lee J, Park YS, Lee CH, Yim JJ, et al. Respiratory virus of severe pneumonia in South Korea: prevalence and clinical implications. PLoS One 2018;13:e0198902. PMID: 29912989.



6. Sanghavi SK, Bullotta A, Husain S, Rinaldo CR. Clinical evaluation of multiplex real-time PCR panels for rapid detection of respiratory viral infections. J Med Virol 2012;84:162-169. PMID: 22052551.


7. Lee KY. Pneumonia, acute respiratory distress syndrome, and early immune-modulator therapy. Int J Mol Sci 2017;18:E388. PMID: 28208675.

8. Shah RD, Wunderink RG. Viral pneumonia and acute respiratory distress syndrome. Clin Chest Med 2017;38:113-125. PMID: 28159154.


9. Hong HL, Hong SB, Ko GB, Huh JW, Sung H, Do KH, et al. Viral infection is not uncommon in adult patients with severe hospital-acquired pneumonia. PLoS One 2014;9:e95865. PMID: 24752070.



10. Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, et al. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA 2009;302:1872-1879. PMID: 19822627.


11. Jain S, Benoit SR, Skarbinski J, Bramley AM, Finelli L. 2009 Pandemic Influenza A (H1N1) Virus Hospitalizations Investigation Team. Influenza-associated pneumonia among hospitalized patients with 2009 pandemic influenza A (H1N1) virus: United States, 2009. Clin Infect Dis 2012;54:1221-1229. PMID: 22437239.



12. ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012;307:2526-2533. PMID: 22797452.

13. Agarwal R, Aggarwal AN, Gupta D, Behera D, Jindal SK. Etiology and outcomes of pulmonary and extrapulmonary acute lung injury/ARDS in a respiratory ICU in North India. Chest 2006;130:724-729. PMID: 16963669.


14. Buchner J, Mazzeffi M, Kon Z, Menaker J, Rubinson L, Bittle G, et al. Single-center experience with venovenous ECMO for influenza-related ARDS. J Cardiothorac Vasc Anesth 2018;32:1154-1159. PMID: 29325841.


15. Hasvold J, Sjoding M, Pohl K, Cooke C, Hyzy RC. The role of human metapneumovirus in the critically ill adult patient. J Crit Care 2016;31:233-237. PMID: 26572580.


16. Cha MJ, Chung MJ, Lee KS, Kim TJ, Kim TS, Chong S, et al. Clinical features and radiological findings of adenovirus pneumonia associated with progression to acute respiratory distress syndrome: a single center study in 19 adult patients. Korean J Radiol 2016;17:940-949. PMID: 27833410.



17. Choi SH, Huh JW, Hong SB, Lee JY, Kim SH, Sung H, et al. Clinical characteristics and outcomes of severe rhinovirus-associated pneumonia identified by bronchoscopic bronchoalveolar lavage in adults: comparison with severe influenza virus-associated pneumonia. J Clin Virol 2015;62:41-47. PMID: 25542469.


18. Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med 2005;352:1749-1759. PMID: 15858184.


19. Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators. Davies A, Jones D, Bailey M, Beca J, Bellomo R, et al. Extracorporeal membrane oxygenation for 2009 influenza A (H1N1) acute respiratory distress syndrome. JAMA 2009;302:1888-1895. PMID: 19822628.


20. Pham T, Combes A, Roze H, Chevret S, Mercat A, Roch A, et al. Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med 2013;187:276-285. PMID: 23155145.


21. Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med 2014;189:1374-1382. PMID: 24693864.


22. Martin-Loeches I, Schultz MJ, Vincent JL, Alvarez-Lerma F, Bos LD, Sole-Violan J, et al. Increased incidence of co-infection in critically ill patients with influenza. Intensive Care Med 2017;43:48-58. PMID: 27709265.



23. Rozencwajg S, Brechot N, Schmidt M, Hekimian G, Lebreton G, Besset S, et al. Co-infection with influenza-associated acute respiratory distress syndrome requiring extracorporeal membrane oxygenation. Int J Antimicrob Agents 2018;51:427-433. PMID: 29174419.


Figure 1
The number of patients with acute respiratory distress syndrome during the period. ARDS: acute respiratory distress syndrome; RT-PCR: reverse transcription-polymerase chain reaction.
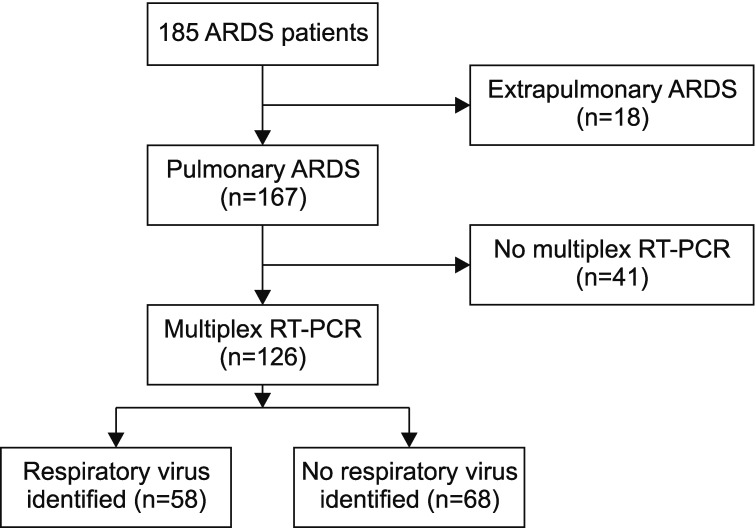
Table 1
Comparison of characteristics between patients with influenza and those with other respiratory virus infection
BMI: body mass index; DM: diabetes mellitus; CHF: chronic heart failure; CKD: chronic kidney disease; CLD: chronic liver disease; CVD: cerebrovascular disease; COPD: chronic obstructive pulmonary disease; APACHE: Acute Physiology and Chronic Health Evaluation; SOFA: Sequential Organ Failure Assessment; AKI: acute kidney injury; RRT: renal replacement therapy; HFNC: high flow nasal cannula; IMV: invasive mechanical ventilation; NM: neuromuscular; ECMO: extracorporenal membrane oxygenation.


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




