 |
 |
| Tuberc Respir Dis > Volume 79(1); 2016 > Article |
|
Abstract
Iron supplements such as ferrous sulfate tablets are usually used to treat iron-deficiency anemia in some elderly patients with primary neurologic disorders or decreased gag reflexes due to stroke, senile dementia, or parkinsonism. While the aspiration of ferrous sulfate is rarely reported, it is a potentially life-threatening condition that can lead to airway necrosis and bronchial stenosis. A detailed history and high suspicion of aspiration are required to avoid delays in diagnosis and treatment. The diagnosis can be confirmed by bronchoscopic examination and a tissue biopsy. Early removal of the aspirated tablet prevents acute complications, such as bronchial necrosis, hemoptysis, and lobar consolidation. Tablet removal is also necessary to prevent late bronchial stenosis. We presented the first case in Korea of a ferrous sulfate tablet aspiration that induced severe endobronchial inflammation.
Foreign body aspiration is a potentially life-threatening medical condition that requires prompt recognition and action 1. Aspiration of chemically active foreign body, such as ferrous sulfate tablet, can lead to granuloma formation and tissue necrosis resulting in bronchial stenosis2.
Although foreign body aspiration is uncommon in adult, the elderly, particularly those with primary neurologic disorders and decreased gag reflexes due to alcohol, seizures, strokes, trauma, senile dementia, and parkinsonism, are also at risk of aspiration3. Furthermore, elderly patients have an increased risk of iron-deficiency anemia which makes them to ingest iron supplements such as ferrous sulfate tablet4.
We describe a case of aspiration of a ferrous sulfate tablet followed by severe endobronchial inflammation.
A 91-year-old woman was admitted to our hospital complaining of cough, sputum, dyspnea, and epigastric discomfort for 1 week. She had a history of early gastric cancer and gastrectomy. She was alert and her vital signs were stable. The physical exam was unremarkable, except for slightly reduced breathing sounds in the right middle and lower lung fields. Routine laboratory tests, including liver and renal function, were normal, other than an elevated erythrocyte sedimentation rate (48 mm/hr) and C-reactive protein level (50.70 mg/L), and a slightly elevated procalcitonin level (0.11 ng/mL).
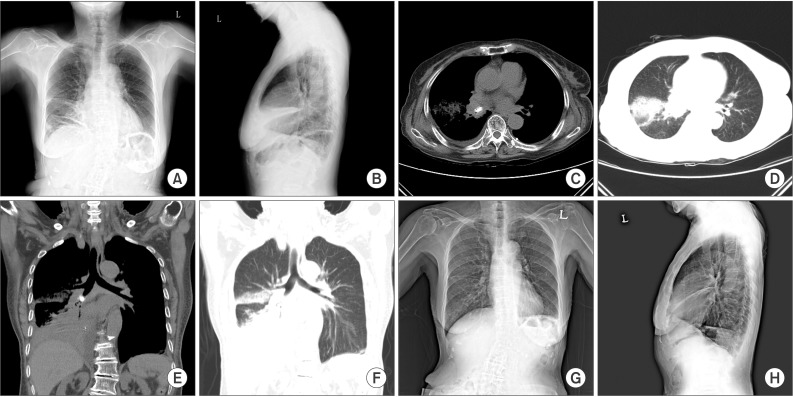
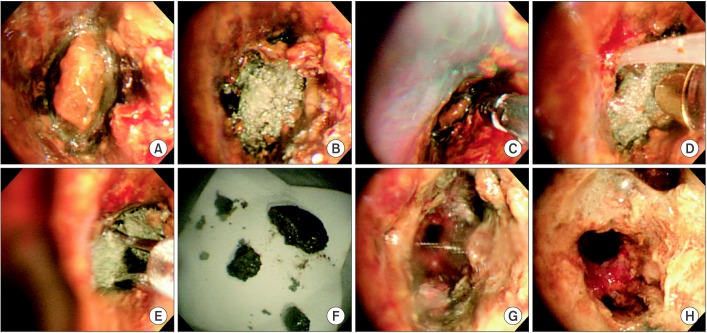
The initial chest X-ray showed atelectasis of the right middle lung and consolidations in the right lower lung, with thickening of the right minor fissure (Figure 1A, B). Under a diagnosis of pneumonia, we initially treated her with intravenous ceftriaxone and clindamycin for 5 days. Chest computed tomography (CT) was performed due to persistent symptoms and showed a high-density lesion in the right bronchus intermedius and atelectasis in the right middle and lower lobes, consolidations and ground-glass opacities in the right upper and lower lobes, and a right pleural effusion (Figure 1C-F). Bronchoscopic evaluation revealed near-total obstruction of the right bronchus intermedius due to impacted pill-like material, which appeared brown to gray in color and fragile in nature. The endobronchial mucosa around the material was yellowish brown, very edematous and inflamed, and friable to the touch with bleeding (Figure 2A, B). The pill-like material was removed using biopsy forceps, W-shaped grasping forceps and a cryotherapy system (Figure 2C-G). Histologically, the tissue around the material revealed chronic inflammation and erosion, with old hemorrhage (Figure 3A-C). On iron staining, hemosiderin granules were identified (Figure 3D).
A detailed history was taken with a suspicion of medication aspiration. She recalled that her initial symptoms developed after ingesting her daily ferrous sulfate tablets. She had been taking them for the last 3 years, to treat iron-deficiency anemia. The tablets were film coated and light brown. We postulated that she had aspirated a ferrous sulfate tablet based on the clinical history, chest CT, bronchoscopic findings, and results of the histological examination.
We started treatment with intravenous methylprednisolone at 1 mg/kg for 7 days. After 1 week, the previous severe endobronchial inflammation of the right bronchus intermedius had improved, but still remained, and the right middle and lower lobar bronchi were patent on bronchoscopic examination (Figure 2H). The steroid was tapered over 4 weeks and her symptoms and chest images resolved (Figure 1G, H).
The aspiration of medication tablets in adults is rarely reported because the tablets are too small to recognize aspiration events and, if recognized, the events often resolve spontaneously with forced expulsion of the tablet. Aspiration of medication tablets manifests in various ways according to their chemical property, if it occurs. For example, alendronate or tetracycline dissolves within the airway producing marked mucosal edema, inflammation and even a pseudomembrane. Aspirated materials were not found on bronchoscopic examination 5,6. On the other hand, non-dissolved medications such as calcium carbonate or ciprofloxacin cause airway obstruction and subsequent obstructive pneumonia rather than airway inflammation. Tablets were pulled out as intact form 7,8. Complications associated with inert tablets were less severe and easily resolved with mechanical extraction9.
Aspiration of a ferrous sulfate tablet is a medical emergency that requires prompt recognition and removal because ferrous sulfate rapidly dissolves within the airway and produces substantial mucosal inflammation, necrosis, and potentially severe bronchial stenosis10,11,12. Clinically, a detailed history is important for diagnosing aspiration of a ferrous sulfate tablet. The symptoms of ferrous sulfate aspiration are non-specific and include coughing, chest discomfort, dyspnea, hemoptysis, and wheezing. Reduced breath sounds with or without wheezing or crackles is the most common physical finding. A chest X-ray may show atelectasis or consolidation. High attenuation lesion on CT may be helpful as in our case. Although evidences are insufficient, iron in ferrous sulfate can be seen as dense opacity like parenchymal iron in siderosis13. The diagnosis can be confirmed by a bronchoscopic examination and tissue biopsy. The common findings are airway inflammation, necrosis, and ulceration of the involved bronchial mucosa10,11,12,14. These finding are caused by the oxidation of ferrous sulfate, resulting in the local production of cytotoxic oxidants and free radicals. Brown necrotic materials are often seen in the acute phase of aspiration15. An intact form of ferrous sulfate tablet is rarely detected because it dissolves quickly. Therefore, a biopsy of the involved mucosa is essential for a correct diagnosis. The histological examination invariably shows staining for ferric iron with surrounding granulation tissue10,14. Aspiration of ferrous sulfate should be treated as soon as possible, otherwise ferrous sulfated-induced airway inflammation may lead to permanent airway stenosis12. Early removal of the aspirated tablet prevents serious complications, such as bronchial necrosis, hemoptysis, and lobar consolidation.
Our patient could not recall the aspiration event at first. Consequently, we did not include ferrous sulfate aspiration in the initial differential diagnosis. However, the clinical unresponsiveness to empirical treatment for pneumonia, high-attenuation lesion on chest CT, pill-like material and severe inflammatory mucosal change with discoloration on bronchoscopic examination, and hemosiderin granules on iron staining on histological examination led us to suspect aspiration of a medication tablet. We confirmed the aspiration of ferrous sulfate after obtaining a detailed medication history. As the diagnosis and treatment were done quickly, she recovered without late complications, such as stenosis.
To the best of our knowledge, this is the first case of aspiration of a ferrous sulfate tablet that induced severe endobronchial inflammation in Korea. A detailed history of aspiration, combined with a bronchoscopic examination and biopsy to investigate specific airway inflammation and staining for iron, are essential for the diagnosis of ferrous sulfate aspiration. Prompt removal of the aspirated tablet is necessary to prevent acute and late complications.
References
1. Baharloo F, Veyckemans F, Francis C, Biettlot MP, Rodenstein DO. Tracheobronchial foreign bodies: presentation and management in children and adults. Chest 1999;115:1357-1362. PMID: 10334153.


2. Lamaze R, Trechot P, Martinet Y. Bronchial necrosis and granuloma induced by the aspiration of a tablet of ferrous sulphate. Eur Respir J 1994;7:1710-1711. PMID: 7995402.


3. Boyd M, Watkins F, Singh S, Haponik E, Chatterjee A, Conforti J, et al. Prevalence of flexible bronchoscopic removal of foreign bodies in the advanced elderly. Age Ageing 2009;38:396-400. PMID: 19401339.



4. Lee JO, Lee JH, Ahn S, Kim JW, Chang H, Kim YJ, et al. Prevalence and risk factors for iron deficiency anemia in the korean population: results of the fifth KoreaNational Health and Nutrition Examination Survey. J Korean Med Sci 2014;29:224-229. PMID: 24550649.



5. Mahmood K, Koubar S, Shofer SL, Ninan NA, Wahidi MM. Alendronate tracheobronchitis. Ann Am Thorac Soc 2013;10:64-66. PMID: 23509337.


6. Sundar KM, Elliott CG, Thomsen GE. Tetracycline aspiration: case report and review of the literature. Respiration 2001;68:416-419. PMID: 11464092.


7. Karakan Y, Akpinar A, Yildiz H, Aksoy H, Dikensoy O. A case of ciprofloxacin tablet aspiration. Tuberk Toraks 2010;58:97-99. PMID: 20517737.

8. Micallef J, Montefort S, Mallia Azzopardi C, Galea J. Two cases of aspiration of calcium tablets. Lung India 2011;28:312-314. PMID: 22084552.



9. Radiological notes: aspirated capsule in right lower lobe. J Mt Sinai Hosp N Y 1966;33:530-532. PMID: 5225499.

10. Cimino-Mathews A, Illei PB. Cytologic and histologic findings of iron pill-induced injury of the lower respiratory tract. Diagn Cytopathol 2013;41:901-903. PMID: 22508539.


11. Maw M, Chiu R, Lim AY. Bronchoscopic and histological changes over time following acute ferrous sulphate tablet aspiration. BMJ Case Rep 2012;2012:bcr2012007329.



12. Venci NM, Watson TJ, Kallay MC. Bronchial stenosis following ferrous sulfate aspiration: case report and review of the literature. J Bronchology Interv Pulmonol 2014;21:58-60. PMID: 24419189.


13. Ceylan N, Bayraktaroglu S, Savas R, Alper H. CT findings of high-attenuation pulmonary abnormalities. Insights Imaging 2010;1:287-292. PMID: 22347923.




14. Lee P, Culver DA, Farver C, Mehta AC. Syndrome of iron pill aspiration. Chest 2002;121:1355-1357. PMID: 11948075.


15. Kim ST, Kaisar OM, Clarke BE, Vandenburg RA, Allen DH, Bell SC, et al. 'Iron lung': distinctive bronchoscopic features of acute iron tablet aspiration. Respirology 2003;8:541-543. PMID: 14708558.


Figure┬Ā1
(A, B) The admission chest X-ray showed atelectasis of the right middle lung and consolidations of the right lower lung, with thickening of the right minor fissure: posteroanterior (A) and lateral views (B). (C-F) Chest computed tomography on hospital day 5 showed a high-density lesion in the right bronchus intermedius, atelectasis in right middle and lower lobes, consolidations and ground-glass opacities in the right upper and lower lobes, and a right pleural effusion: mediastinal (C, E) and lung (D, F) settings. (G, H) Chest X-ray 1 month after the end of treatment showed near-complete resolution of the lung lesions seen on admission.
Figure┬Ā2
(A, B) The bronchoscopic examination showed near-total obstruction of the right bronchus intermedius due to impacted pill-like material, which appeared greyish brown and fragile. The endobronchial mucosa around this material showed severe edematous inflammatory and friable changes, with a touch bleeding and yellowish brown discoloration. (C-G) Procedure images showing removal of the pill-like material with grasp biopsy forceps, W-shaped grasping forceps, and a cryotherapy system with grasp biopsy forceps (C), with the cryotherapy system (D), with W-shaped grasping forceps (E), removed pill-like materials (F), and right bronchus intermedius after removal (G). (H) Bronchoscopic examination 1 week after removing the tablet showed that the previous severe endobronchial inflammation of the right bronchus intermedius was improved, but still remained.
Figure┬Ā3
(A-D) The pathological results of the removed pill-like material and biopsy tissue around the pill-like material in the right bronchus intermedius revealed aspiration of ferrous sulfate. (A) Removed pill-like material. (B) Bronchus intermedius (A and B, H&E stain, ├Ś100; C, H&E stain, ├Ś400; D, iron stain, ├Ś400).



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




