The Need for a Well-Organized, Video-Assisted Asthma Education Program at Korean Primary Care Clinics
Article information
Abstract
Background
The purpose of this study was to assess the effect of our new video-assisted asthma education program on patients' knowledge regarding asthma and asthma control.
Methods
Adult asthmatics who were diagnosed by primary care physicians and followed for at least 1 year were educated via smart devices and pamphlets. The education sessions were carried out three times at 2-week intervals. Each education period lasted at most 5 minutes. The effectiveness was then evaluated using questionnaires and an asthma control test (ACT).
Results
The study enrolled 144 patients (mean age, 56.7±16.7 years). Half of the patients had not been taught how to use their inhalers. After participating in the education program, the participants' understanding of asthma improved significantly across all six items of a questionnaire assessing their general knowledge of asthma. The proportion of patients who made errors while manipulating their inhalers was reduced to less than 10%. The ACT score increased from 16.6±4.6 to 20.0±3.9 (p<0.001). The number of asthmatics whose ACT score was at least 20 increased from 45 (33.3%) to 93 (65.3%) (p<0.001). The magnitude of improvement in the ACT score did not differ between patients who received an education session at least three times within 1 year and those who had not. The majority of patients agreed to the need for an education program (95.8%) and showed a willingness to pay an additional cost for the education (81.9%).
Conclusion
This study indicated that our newly developed education program would become an effective component of asthma management in primary care clinics.
Introduction
Asthma is a major chronic inflammatory airway disease that often occurs with chronic obstructive pulmonary disease (COPD)1. The objective of asthma treatment is to maintain control of asthma symptoms and prevent acute exacerbations. To achieve this goal, the Global Initiative for Asthma document has consistently recommended asthma management using corticosteroid inhalers as the first-line therapeutic option1. However, despite significant progress in asthma management, a substantial proportion of asthmatics still do not achieve adequate control2. Inappropriate prescriptions as well as an insufficient understanding of asthma and incorrect use of inhalers are well-known causes of this lack of control. A systematic review showed 24%–69% of asthmatics used their prescribed inhaled corticosteroids (ICSs) less than half of the time2. Therefore, physicians should make efforts to help asthmatics adhere to their medications and update their knowledge of asthma. Additionally, since many studies have revealed that education programs improve compliance to medication and inhalation techniques2345, an organized education program should also be prepared.
According to the Health Insurance Review and Assessment Service (HIRA), inhalers for asthma or COPD are prescribed at primary care clinics in Korea at a rate of <20%6. In contrast, the rate of hospitalization due to asthma in Korea has been reported to be higher than that in developed countries6, which could indicate that asthma management at primary care clinics is not sufficient or optimal. Several important reasons that may explain these results are the Korean health insurance system and the absence of a well-organized asthma management program. In 2016, the health insurance system of Korea still does not support asthma education, including training on the proper inhaler technique. As a result, most physicians or hospitals are unwilling to provide education associated with asthma.
Recently, the Korean Academy of Tuberculosis and Respiratory Diseases (KATRD) investigated the degree of knowledge about asthma in both primary physicians and asthmatics and also the management status of primary care clinics using a newly developed questionnaire survey. At the same time, an organized, video-assisted education program was provided in collaboration with AstraZeneca Korea using smart devices. With these programs, we tried to investigate the actual conditions of asthma education and also assess the effect of our new education program on asthma control and improvement of patients' knowledge about asthma.
Materials and Methods
1. Inclusion and exclusion criteria
Participants from 43 primary care clinics aged ≥20 years who had been diagnosed with asthma by their primary care physicians were screened. All participants provided written informed consent. Asthmatics with severe heart or renal diseases, bronchiectasis, a transplanted organ, or sequelae of pulmonary tuberculosis were excluded. Patients who had been diagnosed with COPD by their physicians, were pregnant or refused to provide informed consent were also excluded.
2. Study design
To compare the outcomes both before and after our education program, we recruited prospective asthmatics from seven provinces in Korea who had visited their primary care clinics. The study protocol was reviewed and approved by the Inje University Institutional Review Board. A video and pamphlet-based, organized education program was provided to patients who had been regularly managed at each primary care clinic for at least 1 year. The definition of regular management at primary care clinics was defined as a hospital visit at least three times within 1 year. In addition, the physicians at the primary care clinics were educated using the pamphlets developed for our program.
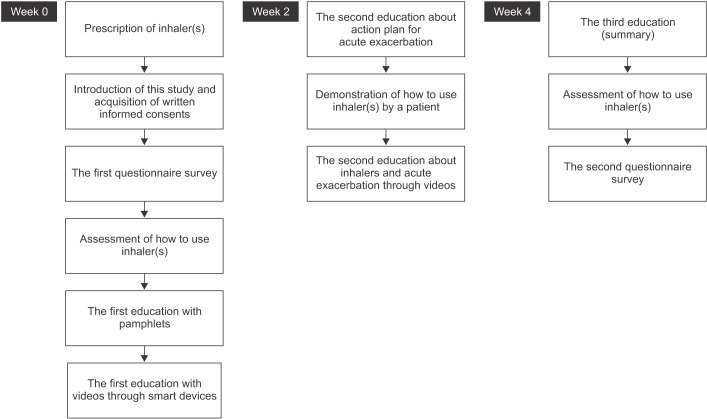
The asthmatics who were enrolled were scheduled for three educational visits in 1 month (Figure 1). In week 0, their baseline knowledge of asthma was assessed using questionnaires, and their methods of inhaler use were also tested after the participants provided informed consent. Thereafter, the first education session about asthma itself and how to use their inhalers was started with key message education using pamphlets. This education was reinforced by having the participants watch videos on a smart device. The patients visited their clinics 2 weeks later (week 2) for the second education session. During week 2, patients were given an action plan for acute exacerbations. Their physicians also observed how they used their inhalers. After that, video-assisted education sessions on acute exacerbations and inhalation techniques were conducted. In the fourth week (week 4), all of the information about asthma was reviewed via videos and was also refreshed by the physicians. Additionally, patients gave a demonstration of how to use their inhalers. Shortly thereafter, the second questionnaire was administered. It included the participants' degree of satisfaction with the education program, their knowledge of asthma, their asthma control test (ACT) score, and questions about each step of inhaler use, which had five, seven, six, and three items, respectively. The minimum clinically important difference (MCID) of the ACT score was defined as three points7. The duration of the education session at each visit was 5 minutes or less. The patients were educated in the waiting room of each clinic.
3. Statistical methods
Statistical analysis was conducted using the SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). All data are displayed as the mean and standard deviation. For continuous variables, the results were presented as the number (%) of cases in each category. Paired t test and chi-square tests were performed with significance set at 0.05 for the comparison between pre-education and posteducation and also between subgroups.
Results
1. Baseline characteristics of the study population and primary care clinics
This study enrolled 144 asthmatics from 28 of 43 primary care clinics which screened patients with asthma (Table 1). The proportion of females was higher (58.3%) than the number of males. The mean age was 56.7±16.7 years. The most common comorbidity was hypertension (37.5%). The inhaler that patients had the most experience with was the Diskus. The patients had received education about asthma at a frequency of 1.74±1.08 times per year. However, nearly 60% of the patients had received no education in the past year; half of the patients had not been taught how to use their inhalers. Less than one-fifth of the patients received asthma education whenever they visited their clinics.
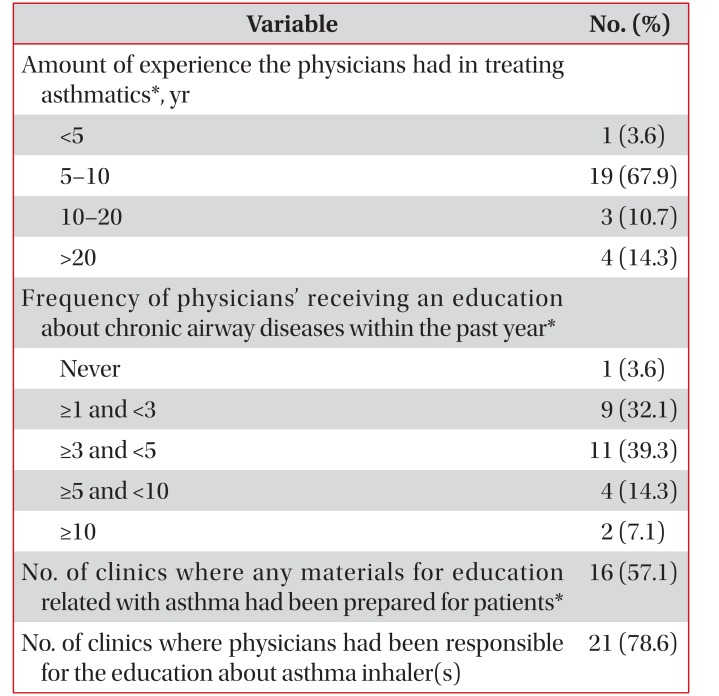
Most physicians at primary care clinics (96.4%) had followed their asthmatics for 5 years or more and had received education about chronic airway diseases at least once a year (Table 2). Although three-fourths of the physicians had taught their patients how to use their inhalers, 42.9% of primary care clinics did not have any materials for education that were specific for asthma that could be distributed to patients.
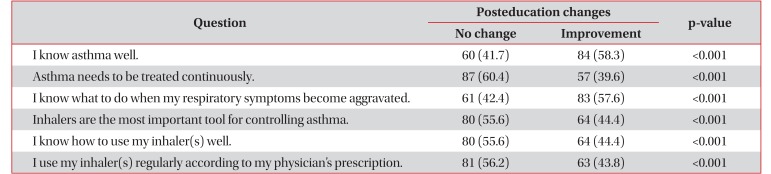
2. Changes in the degree of understanding of asthma after education
The questionnaire about knowledge of asthma included six questions (Table 3). The answers for each question consisted of a four-grade answer scale (strongly disagree, weakly disagree, weakly agree, and strongly agree). The patients selected one of the four answer choices. Improvement was defined as any change (at least one grade) toward a more positive answer after receiving the education. The knowledge associated with asthma improved in 39.6%–58.3% of patients following the education sessions. These changes were all statistically significant (p<0.001 for all questions).
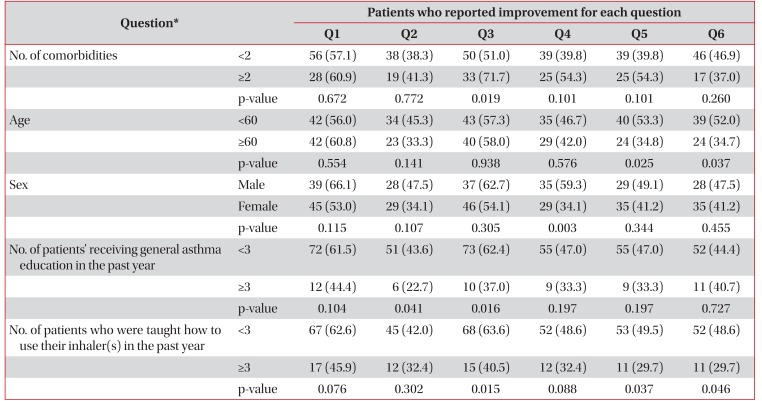
Table 4 demonstrates the number (percentage) of patients who responded with “improvement” to each question after the education according to the patients' clinical characteristics. Regardless of the number of underlying diseases, age and sex, improvement was observed at a similar rate for nearly all the questions. We also could identify “improvement” even in the patients (22.7%–45.9% in all questions) with a history of more than three education sessions in the past year, although patients with a lower frequency of education about asthma or the usage of their inhalers showed a greater effect of education.
3. Changes in the usage of inhalers between the pre-education and posteducation
The physicians assessed seven steps related with inhaler use both before and after the education. The degree of performance in each step was originally evaluated according to a four-grade scale (worst, bad, good, and excellent). “Can do” at each step was defined when the degree of performance was rated as “good” or “excellent.” In contrast, “Can't do” was designated when the responses corresponded to “bad” or “worst.” Out of all the patients, 115 could demonstrate how to use their inhalers before the education. The posteducation assessment on the usage of inhalers was available in 118 of the 128 patients. The participants made the least number of errors during the step of opening the lid of the inhaler correctly, whereas the maximal expiration prior to the inspiration step was the one where patients most frequently made errors (Figure 2).

Changes in the patients' ability to use their inhalers between pre-education and posteducation. “Can do” at each step was defined as a degree of performance that was “good” or “excellent,” while “Can't do” was corresponded to “bad” or “worst.” (A) He(She) can open the lid correctly. (B) He(She) can hold the inhaler(s) properly. (C) He(She) exhales enough prior to inhalation. (D) He(She) understands the manner of inhalation, such as the rate of inhalation and timing. (E) He(She) holds his(her) breath for at least 5 seconds after inhalation. (F) He (She) breathes out after removing the inhaler from his(her) mouth. (G) He(She) rinses his(her) mouth after using the inhaler. The number above the bars indicates the number of patient cases.
After receiving the education, the ability to perform each step significantly improved (p<0.001) (Figure 2). In particular, even though over 60% of patients made errors for both maximal exhalation prior to inhalation and holding their breath for at least 5 seconds, the proportion of patients who made errors after the education sessions were conducted was reduced to below 10%.
4. Changes in the ACT scores from pre-education to posteducation
After finishing the education program, the mean ACT score significantly improved from 16.6±4.6 to 20.0±3.9 (p<0.001). This progress was made in the MCID of the ACT score. An increase in the ACT score by three or more points was demonstrated in 50.4% of those who had received general asthma education at least three times within the past year and also in 55.5% of patients who had not (p=0.231). Additionally, the proportion of patients whose ACT score increased by three or more did not differ between patients who had been educated about the inhalation technique at least three times and in those who had not (49.5% vs. 56.7%, respectively; p=0.103) (Figure 3).
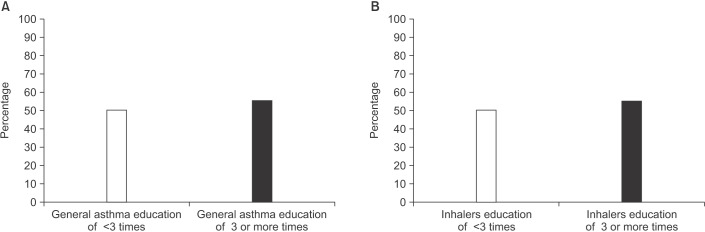
The effects on the proportion of patients who had a posteducation asthma control test score of 20 or more according to the frequency of receiving previous general asthma education (A) and inhaler education (B) within the past year.
Overall, the number of asthmatics with an ACT score ≥20 also increased from 45 (33.3%) to 93 (65.3%) (p<0.001) (Figure 4). In patients who had received general asthma education at least three times, the proportion of patients with an ACT score ≥20 increased from 40.7% to 74.1%. This change was not different from that of patients who had been educated fewer than three times (31.6% to 63.2%, p=0.823). Even in terms of inhaler education, similar results were identified (32.7% to 65.4% in patients with less than three sessions of previous inhaler education vs. 35.1% to 64.9% in those with at least three previous inhaler education sessions, p=0.842). The degree of changes in the ACT scores was also not associated with age, sex, number of comorbidities, or the type of inhaler.
5. Degree of satisfaction, need for education, and willingness to pay an additional cost for the education
Along with an improvement in their overall understanding following the education, most asthmatics (95.8%) agreed with the need for a well-organized education program (Figure 5). In addition, 81.9% of asthmatics showed a willingness to pay for the asthma education.
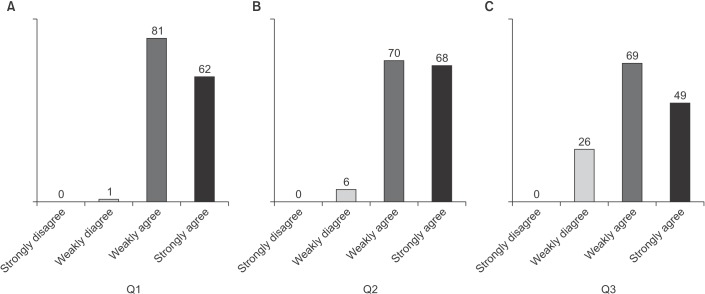
Degree of satisfaction, need for education and willingness to pay an additional cost for the asthma education. (A) Q1: Did you learn more about your disease through the education provided by your clinics? (B) Q2: Do you think an education program like this one should be offered to other patients with your disease? (C) Q3: Would you be willing to receive an education like this despite having to pay an additional cost? The number above the bars indicates the number of cases.
Discussion
Since asthma cannot be cured and its symptoms vary over time and in intensity, the concept of “control” has been used in place of “treatment.” Therefore, one of the goals of asthma treatment is to control its symptoms. As a way to maintain control maximally, several local or international guidelines have been published based upon the accumulated evidence and local situations89. Despite some differences among them, they have commonly emphasized the importance of education regarding asthma and also ICSs as the first-line therapeutic option.
However, although local guidelines in Korean have been disseminated, the prescription rate of ICSs in Korea is still lower than those of European countries and in the United States101112. A recent Korean study reported that the effect of guidelines on the ICS prescription rate was minimal, especially in primary care clinics13. Patients' unawareness or misunderstanding about ICSs as a means to control asthma is one of reasons for the lower rate of ICS prescriptions1415. In addition, although education and verification of inhaler techniques are also crucial for maintaining asthma control16, many physicians do not or cannot educate their patients sufficiently in the real world17. These factors are indicative of the presence of barriers to meeting the recommendations of the guidelines and/or the absence of a well-organized nationwide/communitywide system. Therefore, it is vital to examine the real situation, especially at the primary care level. Furthermore, a well-organized education program specific to a nation or community must be developed and implemented.
The KATRD recently launched a project in collaboration with a multinational pharmaceutical company to develop a teaching program for asthma and also to investigate the actual situation of asthma management at the primary care clinic level. As a result, a 4-week, video-assisted asthma education program using smart devices has been developed. Questionnaires were also created to assess the degree of patients' knowledge regarding asthma and satisfaction with our program. Through these methods, we will examine how primary care clinics manage asthma and what we should do in the future to improve the quality of care.
First, although most physicians at primary care clinics had received education about chronic airway diseases at least once a year, about 43% of clinics were not equipped with any materials to help patients understand their disease or use their inhalers. This trend could indicate that only a simple verbal teaching session had been performed at the office or even that no education at all had been conducted. The finding that 50%–60% of patients had never been educated in the past year in our study also supports this assumption. In addition, our study showed that 16.4%–63.3% of asthmatics did not use their inhalers correctly prior to receiving the education. As reported in several previous studies1819, our study also showed that the maximal exhalation prior to inhalation and holding one's breath after inhalation were the steps where patients most frequently made errors when using their medications. However, after being educated, errors in all steps of manipulating inhalers or inhalation were remarkably reduced, which implies that patients would make fewer errors if a proper and well-organized education session (such as our program) were provided.
Secondly, we found that our education program had a great effect on improving patients' knowledge regarding asthma. After finishing the education, approximately 40%–60% of patients thought that their knowledge about asthma had substantially improved. Moreover, we noted a trend that the magnitude of the effect was greater in patients who had received less education within the past year. Symptoms due to asthma vary over time. Some asthmatics do not experience any respiratory symptoms even without the use of inhalers. Therefore, they do not feel the need for inhalers or for consistent care of their chronic disease. This is one of the major reasons why asthmatics do not visit their clinics or adhere to their medication. As our study showed, our well-organized education program changed patients' cognition regarding asthma considerably. In addition, this change likely will result in improved adherence to medication, consistent asthma management and a better prognosis.
Thirdly, we were able to observe objective improvement in control of asthma after our education session. At the time of enrollment, the baseline mean ACT score was <20, which means that most asthmatics at primary care clinics have not been optimally managed. However, our three educational visits increased the ACT score by >3 (16.6±4.6 to 20.0±3.9), which corresponded to the MCID of the ACT. The number of asthmatics with an ACT score >20 was also significantly increased by 32%. It is particularly noteworthy that even asthmatics who had been educated three or more times within the past year received benefits similar to those who had not. This finding indicates that the existing education programs for asthma do not play a role and new education programs should be developed. Our video-assisted education sessions require only 5 minutes per visit and do not involve any extra space or medical professionals/caregivers. Therefore, we think that our education program could be implemented into a nationwide asthma program.
Lastly, most asthmatics (95.8%) agreed with the need for a well-organized asthma education program for their disease. The majority also showed a willingness to pay an additional cost for this type of education. However, approximately 20% did not agree with having to pay despite recognizing the need for education. These results could indicate that a different institutional policy should be provided at the national or community levels. In fact, any well-organized education program cannot be maintained without financial support, as it is time consuming and requires effort. However, it is unfortunate that the health insurance system of Korea has not provided any financial support for asthma education. This is a significant hurdle to implementing and maintaining an effective asthma education program. Physicians or hospitals will likely be unwilling to allocate additional attention to education without financial support. Considering the fact that an education may reduce the frequency of emergency department or hospital visits202122, institutional support for patient education could actually reduce the total medical costs due to asthma.
There are some limitations of our study. First, no control (non-education) group was used. The absence of a control group may be a limitation in assessing the effect or role of our education program. Secondly, asthmatics in our study were diagnosed by physicians based upon their own judgment without the use of pulmonary function or methacholine provocation testing. Therefore, this study may have included patients who were not actually asthmatics. Thirdly, there could be a blindness bias, which might overestimate the effect of our education. However, a study of this type could not become a substantially blind study. Lastly, we were unable to investigate the long-term effects of our education program due to limitations of the study's design.
In summary, our newly developed, video-assisted, short-duration asthma education program demonstrated a positive effect on the degree of patient knowledge regarding asthma, inhalation technique, control of asthma, and need for asthma education. In addition, the education sessions did not require much time or any extra space. Therefore, we suggest that a nationwide asthma education program similar to ours should be conducted by primary care clinics. Additionally, financial support should be considered to ensure that a well-organized education program is implemented in Korea.
Notes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.