Long-Term Outcomes of Adult Lung Transplantation Recipients: A Single-Center Experience in South Korea
Article information
Abstract
Background
Recently, the number of lung transplants in South Korea has increased. However, the long-term outcome data is limited. In this study, we aimed to investigate the long-term outcomes of adult lung transplantation recipients.
Methods
Among the patients that underwent lung transplantation at a tertiary referral center in South Korea between 2008 and 2017, adults patient who underwent deceased-donor lung transplantation with available follow-up data were enrolled. Their medical records were retrospectively reviewed.
Results
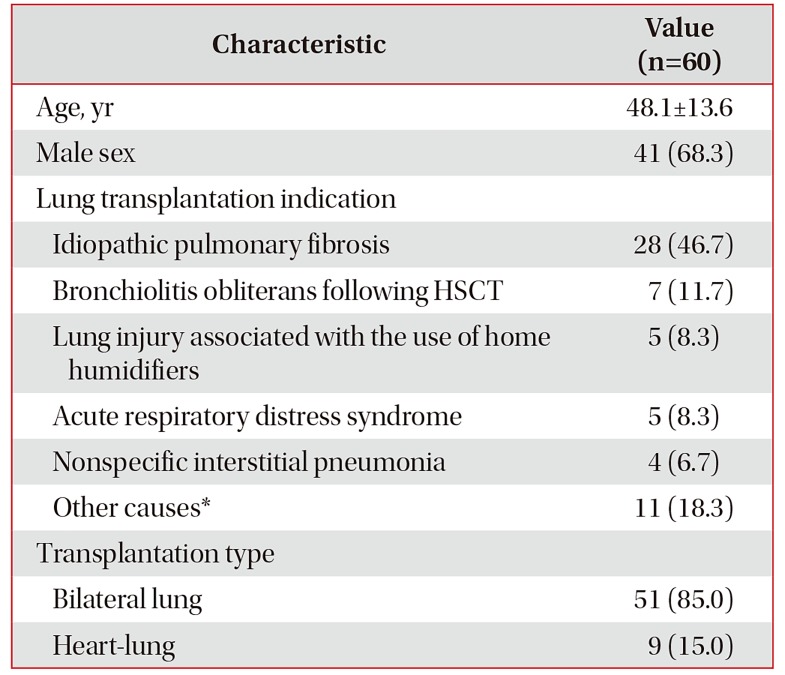
Through eligibility screening, we identified 60 adult patients that underwent lung (n=51) or heart-lung transplantation (n=9) during the observation period. Idiopathic pulmonary fibrosis (46.7%, 28/60) was the most frequent cause of lung transplantation. For all the 60 patients, the median follow-up duration for post-transplantation was 2.6 years (range, 0.01–7.6). During the post-transplantation follow-up period, 19 patients (31.7%) died at a median duration of 194 days. The survival rates were 75.5%, 67.6%, and 61.8% at 1 year, 3 years, and 5 years, respectively. Out of the 60 patients, 8 (13.3%) were diagnosed with chronic lung allograft dysfunction (CLAD), after a mean duration of 3.3±2.8 years post-transplantation. The CLAD development rate was 0%, 17.7%, and 25.8% at 1 year, 3 years, and 5 years, respectively. The most common newly developed post-transplantation comorbidity was the chronic kidney disease (CKD; 54.0%), followed by diabetes mellitus (25.9%).
Conclusion
Among the adult lung transplantation recipients at a South Korea tertiary referral center, the long-term survival rates were favorable. The proportion of patients who developed CLAD was not substantial. CKD was the most common post-transplantation comorbidity.
Introduction
Lung transplantation, an accepted therapeutic method for patients with end-stage lung disease, reportedly results in good functional outcomes and improved quality of life1. However, the development of chronic lung allograft dysfunction (CLAD) limits the long-term survival of these patients. Reportedly, the median survival of lung transplant recipients is only 6.0 years2, which is comparatively lower than that of solid-organ (e.g., liver or kidney) transplant recipients34. Although several efforts have been made to prevent post-lung transplantation CLAD, this complication still occurs in approximately 50% of the patients at approximately 5 years post-transplantation. CLAD is attributable for approximately 30% of deaths occurring between 3 and 5 years post-transplantation5.
According to the official report of the Korean Network for Organ Sharing (KONOS), since the first lung transplantation in South Korea in 1996, the number of cumulative cases of lung transplantation had reached approximately 500 cases by 20176. Since 2013, more than 40 lung transplantations are performed annually in South Korea6.
Several studies have reported the short-term outcomes of lung transplantation, including airway complications, infections, and 1-year mortality789. However, to date, studies reporting on the long-term outcomes of lung transplantation in South Korea are limited10. We, therefore, aimed to investigate the long-term outcomes of lung transplantation recipients at one tertiary referral center, mainly focusing on (1) the survival rates, (2) the development of CLAD, and (3) the incidence of newly developed comorbidities.
Materials and Methods
1. Study subjects
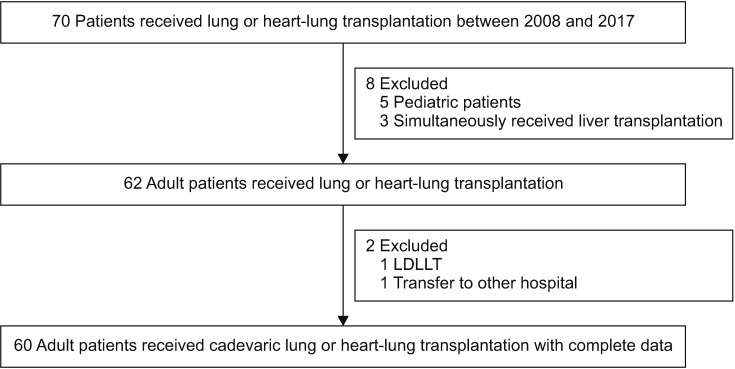
Patients were retrospectively enrolled at Asan Medical Center, which is a 2,700-bed referral hospital in Seoul, South Korea. In 2008, the first lung transplantation was performed at our center. Since then, until December 2017, a total of 70 patients underwent lung transplantation. After excluding (1) pediatric patients, (2) patients who simultaneously received liver transplantation, (3) a patient who underwent a living-donor lobar lung transplantation, and (4) those whose follow-up data were unavailable due to the transfer to another hospital, we retrospectively evaluated the medical records of the remaining patients in November 2018 (Figure 1).
The study protocol was approved by the Institutional Review Board of the Asan Medical Center (IRB No. 2018-0414). The board waived the requirement of informed consent because of the retrospective nature of the analysis.
2. Immunosuppressive therapy protocol
During surgery, patients received induction immunosuppression therapy consisting of basiliximab and a high dose of intravenous methylprednisolone. Post-transplantation, the standard regimen for maintaining immunosuppression was triple therapy comprising steroids, a calcineurin inhibitor, and antimetabolites using prednisone, tacrolimus, and mycophenolate mofetil, respectively. Tacrolimus was adjusted to a target trough level of 10–15 ng/mL for the initial 6 months and 8–12 ng/mL thereafter. Mycophenolate mofetil was initiated at a daily dose of 2 g. The dose was subsequently adjusted to achieve a trough level of 1–3 ng/mL. Additionally, the dose was further adjusted based on the presence of other factors, including the patients' condition, leukopenia, or diarrhea.
3. Infection prophylaxis strategies
Several infection prophylaxis strategies were used8. For antiviral prophylaxis, intravenous ganciclovir was administered at a dose of 5 mg/kg every 24 hours from 1–4 weeks post-transplantation, regardless of the cytomegalovirus serostatus of recipients and donors. Thereafter, oral valganciclovir was administered at a dose of 900 mg once daily until 6 months. For antifungal prophylaxis, voriconazole was intravenously administered at a dose of 4 mg/kg every 12 hours. Once the recipient was able to consume a normal diet, oral voriconazole was administered. The target trough level of voriconazole was 1.5–5.5 mg/dL. If voriconazole was poorly tolerated or adverse effects occurred, voriconazole was replaced by itraconazole. The total duration of antifungal prophylaxis was 6 months. Lastly, oral trimethoprim/sulfamethoxazole, at a dose of 160/800 mg, was administered on alternate days for the recipient's lifetime to prevent pneumonia by Pneumocystis jirovecii.
4. CLAD and prophylactic regimens
We performed pulmonary function tests (PFTs) during outpatient visits (generally, at an interval of 1–3 months) for the diagnosis and functional grading of chronic transplant rejection. As previously defined11, CLAD was diagnosed as a persistent decline in forced expiratory volume in 1 second of at least 20% compared with the two best postoperative values, in absence of other causes. We further differentiated CLAD into bronchiolitis obliterans syndrome (BOS) or restrictive CLAD1213. Because previous studies suggested the role of gastroesophageal reflux disease (GERD) in BOS1415, we prophylactically prescribed a proton pump inhibitor (PPI) therapy (generally, pantoprazole 40 mg once daily) to all patients post-transplantation for lifetime use. Additionally, as the prophylactic drug, azithromycin, is known to prevent BOS16, it was administered at a dose of 250 mg on alternate days to all patients post-transplantation for lifetime use.
5. Analysis for survival, completion rate of infection prophylactic regimen, and cumulative morbidities
Initially, we evaluated survival rates using the Kaplan-Meier method at post-transplantation 1, 3, and 5 years. Further, after identifying the survivors and non-survivors at 1-year, we evaluated the recipients' data, such as demographic characteristics, the use of a mechanical ventilator and/or extracorporeal membrane oxygenation (ECMO) while awaiting transplantation, the preoperative PFT value, and the use of steroids before transplantation, between the two groups to investigate the 1-year survival-related factors. Additionally, we collected the donors' data, such as demographic characteristics, ischemic time, arterial oxygen partial pressure/fractional inspired oxygen ratio, and the cause of death, from the KONOS. Post-transplantation kidney dysfunction was evaluated the need for renal replacement therapy (RRT) after transplantation.
The completion rates of the infection prophylactic regimens and the incidence of newly developed post-transplantation comorbidities, including chronic kidney disease (CKD), diabetes mellitus, hypertension, and hyperlipidemia were investigated, after excluding patients who died within a month post-transplantation.
6. Statistical analysis
Continuous variables were compared using Student's t-test or the Mann-Whitney test, whereas categorical variables were compared using the chi-square or Fisher's exact test. All tests of significance were two-sided, and p<0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 20.0 (IBM Corp., Armonk, NY, USA).
Results
1. Baseline characteristics
Eligibility screening identified 60 adult patients who underwent lung or heart-lung transplantation (Figure 1). A total of 51 patients received bilateral lung transplants because of idiopathic pulmonary fibrosis (n=26), bronchiolitis obliterans following hematopoietic stem cell transplantation (n=7), lung injury associated with home humidifier use (n=4)17, and other diseases (n=14). The remaining nine received bilateral lung-heart transplants because of idiopathic pulmonary fibrosis (n=2), acute respiratory distress syndrome (n=2), and other diseases (n=5). Patients had a mean age of 48.1±13.6 years, and 41 (68.3%) were male. Table 1 shows the age, sex, transplantation type, and the indication for lung transplantation of all patients. A total of 32 patients (53.3%) received ECMO before transplantation with a median duration of 13.5 days (range, 1.0–38.0 days).
2. Post-transplantation survival rates and the cause(s) of death
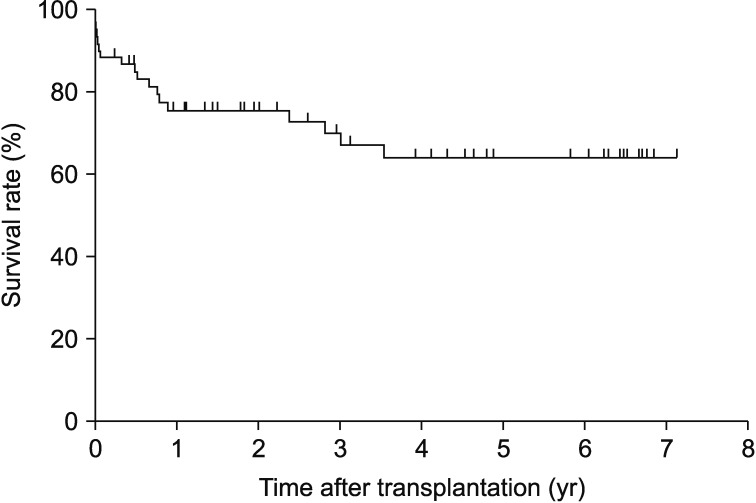
The median follow-up duration post-transplantation was for all 60 patients was 2.6 years (range, 0.01–7.6 years). During the follow-up period, 19 patients (31.7%) died in a median of 194 days (range, 3–1,297 days) after transplantation. Of these 19 patients, 14 patients died within 1-year post-transplantation. The survival rates were 75.5% at 1 year, 67.6% at 3 years, and 61.8% at 5 years. Figure 2 shows the overall survival rates of the 60 patients post-transplantation. The main cause of death within the first year after transplantation was infection (11/14 patients, 78.6%), followed by bleeding (n=3). Past the first year, the causes of death of the remaining five patients included infection (n=3), BOS (n=1), and uremic encephalopathy (n=1).
3. Predictor of 1-year survival
As shown in Table 2, the baseline characteristics of the forty-six 1-year survivors and fourteen 1-year non-survivors were comparable, except for a statistically significant difference in post-transplantation RRT between the two groups. The 1-year non-survivors received post-transplantation RRT more frequently than the survivors (57.1% vs. 6.5%, p<0.001).
4. Acute rejection and CLAD development
A total of four patients (6.7%) were diagnosed with acute rejection among 60 lung transplantation recipients. The median interval between operations and the diagnosis of acute rejection for these four patients was 8.1 months (range, 7.7–28.9 months). Among the four patients, the diagnosis was histopathologically confirmed to be grade A2 acute cellular rejection in one patient only. The diagnosis of the remaining three patients was based on typical radiological findings combined with a dramatic response to treatment with high-dose steroids.
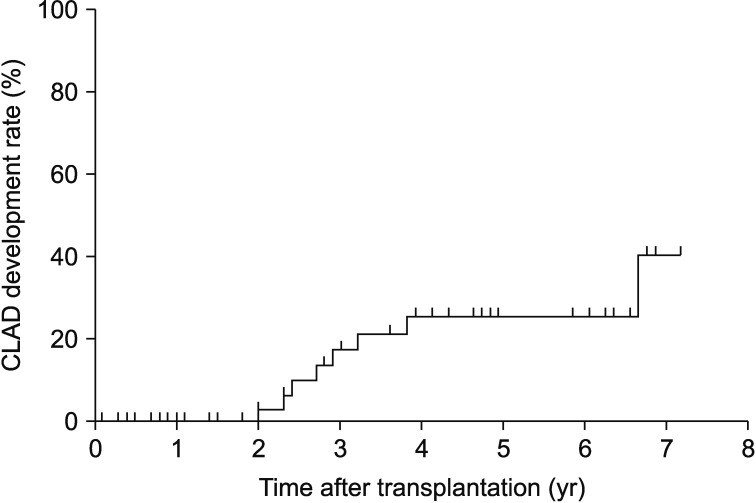
Further, of the 60 patients, eight (13.3%) were diagnosed with CLAD, mostly BOS (n=7), after a mean duration of 3.3±2.8 years post-transplantation. For five patients, CLAD was diagnosed at 1–3 years post-transplantation; for two patients, it was diagnosed at 3–5 years, and for one patient, it was diagnosed more than 5 years after the operation. The CLAD development rate was 0% at 1 year, 17.7% at 3 years, and 25.8% at 5 years. Figure 3 shows the Kaplan-Meier estimates of CLAD development rates.
5. The completion rates of infection prophylactic regimens
After excluding the six patients who died within 1-month post-transplantation, the completion rates of the infection prophylactic regimens were analyzed for the remaining 54 patients. The completion rates of the different regimens were as follows. For antiviral prophylaxis, 31 patients (57.4%) successfully completed a ganciclovir/valganciclovir regimen. A total of 18 patients (33.3%) had to discontinue this treatment because of cytopenia; the remaining five patients discontinued the regimen because of death (n=3), cost (n=1), and vomiting (n=1). For antifungal prophylaxis, 38 patients (70.4%) completed a prophylactic voriconazole regimen without interruption. The most common cause of discontinuation in the remaining patients was visual hallucinations. Oral trimethoprim/sulfamethoxazole was continuously administered to 48 patients (88.9%) without the occurrence of any adverse effects.
6. Incidence of newly developed comorbidities
After excluding the six patients who died within 1-month post-transplantation, the incidence of newly developed comorbidities was investigated for the remaining 54 patients. Among these, various comorbidities developed during a median follow-up time of 2.8 years (range, 0.1–7.6 years). As shown in Table 3, the most common comorbidity was CKD (n=28, 51.9%), which mostly occurred within 1 year after transplantation. Of the 28 patients with CKD, maintenance immunosuppressive regimen was switched to a combination of mammalian target of rapamycin (mTOR) inhibitors and other immunosuppressive agents such as cyclosporine in five patients. The second most common comorbidity was diabetes mellitus (n=14, 25.9%). The Kaplan-Meier estimates for development rates of newly developed comorbidities are shown in Supplementary Figures S1, 2, 3, 4.
Discussion
Although the number of lung transplants has steadily escalated in recent years in South Korea, the literature concerning long-term outcomes, such as survival, rate of CLAD development, and newly developed comorbidities, is limited. Our most important findings were that the long-term survival rates of our subjects were favorable, the proportion of patients who developed CLAD was not substantial, and a substantial portion of patients developed comorbidities, such as CKD or diabetes mellitus, post-transplantation.
We observed a favorable outcome in terms of post-transplantation survival rates. The 1-, 3-, and 5-year survival rates of our study subjects were comparable with those recently reported (82%, 69%, and 59%, respectively) by the International Society for Heart and Lung Transplantation and are remarkably better than those reported by KONOS (60.3%, 50.6%, and 47.9%, respectively) in 2016218. The main difference between our subjects and those of the KONOS registry is that our subjects were consecutive patients from a single center. It was not until the past two consecutive years that our institute performed 10–20 lung transplantation cases per year. Additionally, lung transplantation experience of our center is limited to only 10 years. However, our outcomes are comparable with those of the international registry. We believe that several factors contributed to this favorable outcome: (1) well-defined pre-established protocols in place, (2) prudent selection of deceased donors and recipients, (3) good inter- and multidisciplinary collaboration among the various departments, and (4) the effectiveness of the prophylactic regimens in preventing infection and CLAD. Notably, we have never performed single-lung transplantation, which has a worse survival rate than bilateral transplantation1920.
Among our subjects, the only significant predictor of 1-year survival was post-transplantation RRT. This finding is consistent with the findings of the previous studies92122. One study showed that post-transplantation RRT was associated with increased in-hospital and 1-year mortality22. George et al.21 reported that the requirement of post-transplantation RRT was strongly associated with short- and long-term mortality in 12,108 patients from the United Network for Organ Sharing database. In South Korea, a study from another tertiary referral center reported that needing a post-transplantation RRT was an independent perioperative risk factor for 1-year mortality9. The need for RRT post-transplantation could be considered a state of critical illness9. That is, the patients who develop multiorgan dysfunction post-transplantation are less likely to tolerate medications, showing nephrotoxicity, perioperative hemodynamic instability, and eventually requiring RRT21.
The survival benefits of ECMO use as a bridge for lung transplantation have long been debated. It has been reported that lung transplant recipients undergoing ECMO have increased short- and long-term mortality23, particularly those who receive a transplant after waiting for >14 days24. However, some recent reports showed that a combination of mechanical ventilation and ECMO is a viable bridging strategy, leading to acceptable patient outcomes25. We believe that our subjects were extremely critical wherein approximately 50% of them received ECMO while awaiting transplantation. In contrast, of the >9,000 patients from the United Network for Organ Sharing (UNOS) database between 2005 and 2011, only approximately 1% received ECMO support26. The reason for the high percentage of patients receiving ECMO in our study is related to the Korean lung allocation score criteria, which states that only patients who are connected to a ventilator or ECMO belong to the category status 0 (the most emergent state).
CLAD is the leading cause of death at 1-year post-transplantation13. The International Society for Heart and Lung Transplantation (ISLHT) registry reported that approximately 50% of patients developed BOS within 5 years post-transplantation. In contrast, the incidence of CLAD was lower in our lung transplantation recipients than those in the ISLHT registry. We thought that several factors contributed to lower CLAD development in our subjects. First, immediately after the transplantation, we routinely prescribed PPI to prevent chronic rejection in all patients. GERD induces rejection by triggering a non-allogenic injury to the transplanted lung, and reflux-mediated aspiration is a risk factor for BOS1415. We also routinely administered azithromycin to all patients. This is because one double-blind, placebo-controlled trial showed that prophylactic azithromycin significantly improved BOS-free survival16. The long-term completion rate of these drugs is satisfactory: >90% of our study subjects completed PPI and azithromycin without the occurrence of adverse effects. Second, vast evidence exists of the association of microbial, fungal, and viral colonization/infection with BOS development27. Therefore, our institute's protocol includes the routine prophylactic use of voriconazole and ganciclovir/valganciclovir, which may also help prevent BOS development. However, approximately 50% of our subjects could not complete ganciclovir/valganciclovir prophylaxis.
In our study, we reported the occurrence of various newly developed comorbidities, such as CKD and diabetes mellitus; CKD was the most common comorbidity in our subjects (51.9%), mostly occurring within 1-year post-transplantation. The incidence of CKD development (51.9%) during a median follow-up of 2.8 years is comparable with the incidence of CKD development (55%) reported in an international registry28. CKD development after transplantation is generally attributed to chronic calcineurin inhibitor nephrotoxicity29. Tacrolimus is also known to be associated with the development of comorbidities such as post-transplantation diabetes mellitus, hypertension, and hyperlipidemia30. For patients with kidney dysfunction, adding an mTOR inhibitor and reducing the calcineurin inhibitor dose has shown to improve kidney function313233. Of the 28 patients with CKD in our study, some patients were switched to the administration of sirolimus and cyclosporine to prevent CKD progression.
A limitation of our study was that it was a single-center retrospective review with a limited number of patients. Thus, our study population is probably not completely representative of the lung transplant recipient population in South Korea. Further, our relatively short follow-up period could not adequately reveal the long-term adverse effects.
In conclusion, for adult lung transplant recipients in a tertiary referral center in South Korea, the long-term survival rates are favorable and the rate of CLAD development was not substantial. CKD was the most common newly developed comorbidity post-transplantation, and it occurred mostly within 1-year post-transplantation.
Notes
Authors' Contributions:
Conceptualization: Jo KW, Park SI, Shim TS.
Methodology: Jo KW, Park SI, Shim TS.
Formal analysis: Jo KW, Shim TS.
Data curation: Jo KW, Hong SB, Kim DK, Jung SH, Kim HR, Choi SH, Lee GD, Lee SO, Do KH, Chae EJ, Choi IC, Choi DK, Kim IO
Validation: Jo KW, Hong SB.
Investigation: Jo KW, Park SI, Shim TS.
Writing - original draft preparation: Jo KW, Park SI, Shim TS.
Writing - review and editing: Jo KW, Park SI, Shim TS.
Approval of final manuscript: all authors.
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
Funding: No funding to declare.
References
Supplementary Material
Supplementary material can be found in the journal homepage (http://www.e-trd.org).
Supplementary Figure S1. Kaplan-Meier estimates for chronic kidney disease development of 54 patients who underwent lung transplantation.
Supplementary Figure S2. Kaplan-Meier estimates for diabetes mellitus development of 54 patients who underwent lung transplantation.
Supplementary Figure S3. Kaplan-Meier estimates for hyperlipidemia development of 54 patients who underwent lung transplantation.
Supplementary Figure S4. Kaplan-Meier estimates for hypertension development of 54 patients who underwent lung transplantation.
Supplementary Figure S1
Kaplan-Meier estimates for chronic kidney disease (CKD) development of 54 patients who underwent lung transplantation.
Supplementary Figure S2
Kaplan-Meier estimates for diabetes mellitus development of 54 patients who underwent lung transplantation.
Supplementary Figure S3
Kaplan-Meier estimates for hyperlipidemia development of 54 patients who underwent lung transplantation.
Supplementary Figure S4
Kaplan-Meier estimates for hypertension development of 54 patients who underwent lung transplantation.