Host Blood Transcriptional Signatures as Candidate Biomarkers for Predicting Progression to Active Tuberculosis
Article information
Abstract
A recent understanding of the dynamic continuous spectrum of Mycobacterium tuberculosis infection has led to the recognition of incipient tuberculosis, which refers to the latent infection state that has begun to progress to active tuberculosis. The importance of early detection of these individuals with a high-risk of progression to active tuberculosis is emphasized to efficiently implement targeted tuberculosis preventive therapy. However, the tuberculin skin test or interferon-γ release assay, which is currently used for the diagnosis of latent tuberculosis infection, does not aid in the prediction of the risk of progression to active tuberculosis. Thus, a novel test is urgently needed. Recently, simultaneous and systematic analysis of differentially expressed genes using a high-throughput platform has enabled the discovery of key genes that may serve potential biomarkers for the diagnosis or prognosis of diseases. This host transcriptional investigation has been extended to the field of tuberculosis, providing promising results. The present review focuses on recent progress and challenges in the field of blood transcriptional signatures to predict progression to active tuberculosis.
Introduction
Mycobacterium tuberculosis (MTB), which has coexisted with human for thousands of years [1] and causes tuberculosis (TB), remains an unresolved global health challenge [2,3]. According to the 2021 World Health Organization (WHO) Global TB Report, 2020 milestones of the “End-TB” strategy were mostly not achieved worldwide due to rise in TB deaths and slowing of TB incidence decline [2]. Understanding the natural history of MTB infection should precede effective strategies for successful eradication of MTB. Individuals infected with MTB exhibit different clinical outcomes, depending on the interaction between MTB and host immunity [4,5]. Most of them successfully contain MTB and maintain the status of latent infection using an effective immune response, which is the so-called latent TB infection (LTBI) [4-6]. Individuals with LTBI, accounting for approximately one-fourth of the world’s population [7,8], represent a potential reservoir for active TB because a disrupted equilibrium between MTB and host immunity may cause progression to active TB in 10% of them during their lifetime [9]. Thus, to achieve the goal of the “End-TB” strategy, early identification and treatment of both active TB and LTBI at a high-risk of progression to active TB is clearly critical.
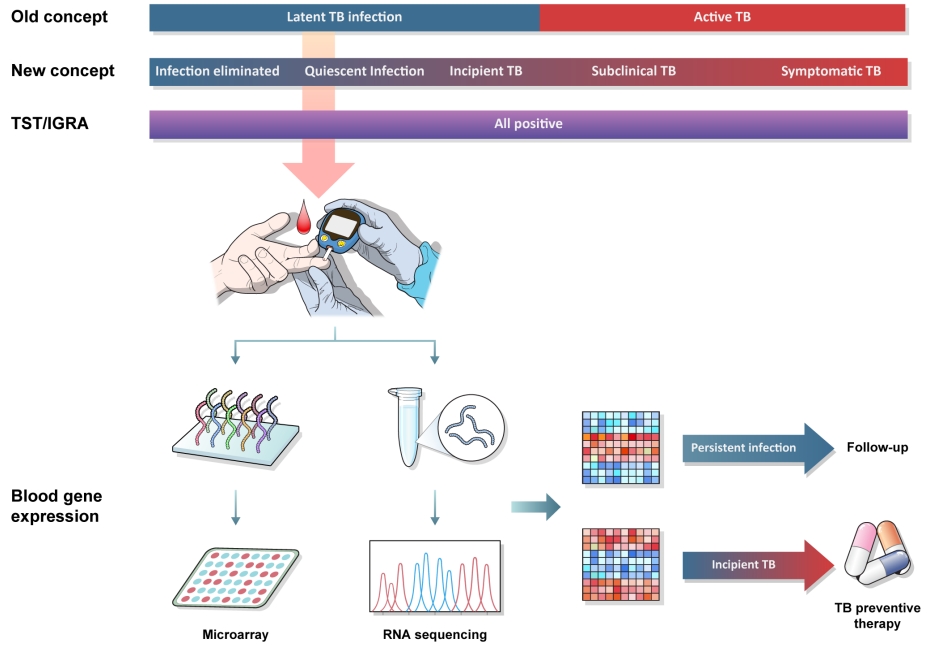
Recent evidence suggests that there is no clear distinction between active TB and LTBI, and the clinical outcomes after MTB infection rather span a continuous spectrum (Figure 1) [9-12]. As there are different disease statuses of active TB, such as subclinical TB or symptomatic TB, LTBI also encompasses a heterogeneous range of infection status [13-15]. In particular, growing evidence indicates the importance of early detection of incipient TB, in which progression to active TB disease has begun but symptoms and radiographic abnormalities have not yet developed [11,16,17]. Individuals with incipient TB are likely to develop active TB within a short time and would benefit most from TB preventive therapy [16,17]. However, a validated test for predicting progression to active TB is not yet available. Recently, biomarker-based approaches including interferon-γ (IFN-γ) response of CD4/CD8 T-cell stimulated with additional MTB-specific peptides, T-cell phenotyping, proteomics, and transcriptomics, have led to incremental improvements in this field [11,18-22]. In particular, several mRNA signatures identified in blood transcriptomic studies have shown promise and are in the most advanced stages of development [22-29]. In this review, we discuss the recent progress and challenges in the field of host blood transcriptional signatures to identify predictive biomarkers for the progression to TB.
Currently Available Diagnostic Tests for LTBI
The diagnosis of LTBI is based on immunological evidence to MTB antigen using the tuberculin skin test (TST) or IFN-γ release assay (IGRA), which cannot differentiate between active TB and LTBI [5]. People with a positive TST or IGRA include those who are successfully cleared from MTB infection and those at high-risk of developing TB in the near future [30]. The positive predictive value (PPV) of TST and IGRA for the development of active TB within 2 years is estimated to be 1% to 4% and the number needed to treat (NNT) in preventing one active TB case is 67–250 for TST and 37–85 for IGRA [22,31-33]. Thus, the search for a novel biomarker that can reflect the heterogeneous status of LTBI on a continuous spectrum and predict risk for future development of TB is urgently necessary, and such biomarker-based TB preventive therapy would help reduce NNT and overcome barriers during implementation of TB preventive therapy [34]. In addition, a big challenge is that TST or IGRA remains positive after TB preventive therapy in individuals with LTBI. A novel test that can monitor the effect of TB preventive therapy will help advance interventions for TB control. In 2017, WHO announced the urgent need to develop a new test to detect the presence of incipient TB and provided target product profiles (TPP), including details on the minimum and optimal performance criteria of the relevant predictive tests for future risk over a specified duration of 2 years [16].
Host Transcriptional Signatures for Predicting Progression to Active TB
1. Basic principle
Gene expression is the process by which information stored in the DNA is converted into a functional product through transcription and translation [35]. Changes in mRNA expression, such as overexpression or underexpression of hundreds or thousands of genes, occur as a transcriptional response to different external stimuli in human pathophysiological conditions [35-37]. Simultaneous and systematic analysis of differentially expressed genes using microarray or RNA sequencing platforms has improved our understanding of the complex pathogenesis of various human diseases and the discovery of key genes with altered expression which may be potential biomarkers for the diagnosis and prognosis of diseases [38]. This host transcriptional investigation has been adopted in infectious diseases and has allowed the simultaneous evaluation of complex interactions between the host and pathogen [35].
Various types of biological materials, including tissue specimens, cells, and blood samples, can be used for gene transcriptional profiling. Peripheral blood, which provides information about the cumulative host immune response throughout the entire body, is an easily accessible and reproducible sample for measuring gene expression [39]. Thus, blood-derived transcriptional analysis has been extensively studied in patients with infectious diseases, including TB [35,39]. Serial blood sampling may enable the tracing of dynamic changes in gene expression over time after infection [37].
Although infectious diseases are generally diagnosed via the detection of pathogens, direct pathogen detection is not always feasible in individuals with different statuses of MTB infection on a continuous spectrum. Given that blood-based host RNA signatures would be reflective of disease state, a consequence of dynamic changes in the immunological equilibrium between MTB and the host, recent clinical studies have focused on a transcriptomic approach for the development of novel TB diagnostic tests (Figure 1) [35]. This approach may be more helpful in diagnosing incipient or subclinical TB, in which MTB detection is more challenging owing to a paucibacillary state, as opposed to symptomatic active TB.
2. Overview of transcriptomic studies for the prediction of progression to active TB
The first large-scale blood transcriptomic study by Berry et al. [40] was heralded as a breakthrough discovery of a promising biomarker for the diagnosis of active TB. They identified a distinct 393-transcript signature dominated by interferon inducible genes from the whole blood of patients with active TB and a subset of individuals with LTBI. The possibility that a blood transcriptional signature may identify incipient TB has been suggested [40]. This study was followed by the extended application of the transcriptomic approach in predicting future incident TB and treatment response monitoring [41-44]. Recent major studies focusing on the blood transcriptome of individuals at high-risk of future development of TB, the population of interest for this review, are summarized in Table 1. The ultimate aim of these studies was to develop a novel blood mRNA signature for the prediction of future TB development and validate its efficacy in different settings.

Summary of recent studies on blood transcriptional mRNA signatures for the prediction of progression to active tuberculosis
In the first stage, candidate TB risk signatures are determined by mining enormous gene expression profiles generated through high-throughput platforms (RNA sequencing or microarray) in a large prospective cohort of individuals with LTBI or a nested case-control study population [23,24]. The RNA signatures identified in the first stage are tested and validated in independent settings using a more targeted quantitative real-time polymerase chain reaction (qRT-PCR) platform [23,24]. Using this strategy, the Zak16 signature (comprised of 16-transcripts: ANKRD22, APLO1, BATF2, ETV7, FCGR1A, FCGR1B, GBP1, GBP2, GBP4, GBP5, SCARF1, SEPT4, SERPING1, STAT1, TAP1, and TRAFD1) was identified in the South African non-human immunodeficiency virus (HIV) adolescent LTBI cohorts. The qRT-PCR based Zak16 signature was independently validated in South African and Gambian non-HIV adult household contact cohorts showing promising performance in predicting TB progression (area under the receiver operating characteristic curve [AUC], 0.72) 12 months preceding TB diagnosis [23]. However, the sensitivity of the Zak16 signature decreased as the time interval before active TB diagnosis increased. A subsequent study conducted in African non-HIV adult household contact cohorts found a novel RISK4 (also known as Suliman4) signature (two upregulated genes, GAS6 and SEPT4 and two downregulated genes, CD1C and BLK) with a modest AUC of 0.66 for TB progression 12 months prior to diagnosis. The AUC was comparatively lower because probably patients who developed active TB within 3 months of enrollment were excluded from the analysis [24].
Another way to develop predictive novel RNA signatures is to use candidate gene signatures previously identified for the diagnosis of active TB, and test or evaluate its performance for the detection of incipient TB in the combined transcriptomic datasets derived from previously published studies or independent cohorts. Significant gene signatures validated or discovered by this approach included BATF2, Roe3, Sweeney3, Gliddon3, Suliman4, and other signatures (Table 1) [25,26]. As opposed to studies of Zak16 and RISK4 signatures to assess diagnostic performance for up to 24 months before TB diagnosis, Roe3 signature was focused on the short-term risk of progression to TB. Although there was a low frequency of progression to TB in the HIV-negative UK TB contacts cohort, the study demonstrated that the Roe3 signature provided a higher PPV for progression to TB than the IGRA (up to 50% vs. 5.6%), suggesting a promising role of blood gene signatures for short-term risk stratification of TB contracts [26]. Similarly, a systematic review identified eight RNA signatures (BATF2, Gliddon3, Kaforou25, Roe3, Suliman2, Suliman4, Sweeney3, and Zak16) with equivalent diagnostic performance for incipient TB over 24 months (AUC, 0.70 to 0.77) and revealed that their performance improved as the time interval before the onset of TB decreased [25].
Despite encouraging results in these studies, whether the implementation of TB preventive therapy in the blood RNA transcript-guided target population would efficiently reduce incident TB is highly important. In this regard, a recent randomized controlled study was conducted to evaluate the efficacy of the RISK11 signature (a simplified 11-gene signature derived from the Zak16 signature)-based TB preventive therapy in HIV-negative community settings in South Africa [27]. Unfortunately, RISK11 signature-based TB preventive therapy with once-weekly doses of isoniazid and rifapentine for 3 months (3HP) failed to reduce TB incidence over 15 months. The possibility that the 3HP regimen was insufficient to sterilize incipient TB detected using this strategy was suggested [27].
Although none of the blood gene signatures hitherto achieved the minimum criteria of the WHO TPP for predicting incident TB within 2 years prior to diagnosis, a promising role for short-term risk prediction was consistently observed (AUC >0.95) [26,27]. The latest headto-head comparison study using eight parsimonious blood transcriptomic signatures (Francisco2, DIAG4, RISK6, RISK4, BATF2, Roe3, Sweeney3, and Thompson5) and RISK11 reaffirmed this finding [45]. Most of the eight RNA signatures met the minimal WHO target criteria within 6 months prior to TB diagnosis. In particular, the RISK11 signature achieved the optimal target criteria for predicting TB progression over 6 months.
Additionally, the predictive performance of the blood transcriptional signature for incident TB did not decline in people living with HIV (PLHIV) [28]. Thus, the application of community-based transcriptomic testing once or twice a year would be feasible as a TB preventive strategy for PLHIV in areas with high TB prevalence [28].
Finally, efforts to develop a point-of-care testing platform with more refined transcriptomic signatures have already been done, although studies have mostly been conducted in terms of a triage or a diagnostic test for active TB, rather than an incipient TB test [29,42]. A recent study using the Cepheid MTB Host Response cartridge with fingerpricked blood samples, applying the Sweeney3-gene signature, showed promising performance as a point-of-care triage test for active TB [29]. TB score based on mRNA expression of three genes (GBP5, DUSP3, and KLF2) discriminated between active TB and other respiratory diseases with an AUC of 0.94 (95% confidence interval [CI], 0.91 to 0.97) when evaluated against GeneXpert Ultra (Cepheid, Sunnyvale, CA, USA). When the sensitivity was set at 90% for the triage test, the specificity was 86% (95% CI, 75% to 97%). The results were not influenced by the geographic area or HIV infection status. These interim data reached the WHO minimal TPP for a point-of-care triage test for TB, although this study was conducted in adult patients presenting with symptoms suggestive of TB with a small sample size and subgroups. However, early gene expression changes during infection progression prior to the development of active TB may be subtle compared with those in overt active TB. Thus, the performance of the gene signature in predicting TB progression is likely less accurate than that in discriminating between individuals with active TB and healthy controls or those with other respiratory diseases.
3. Challenges
Most studies were performed in specific regions, such as Africa and the UK. The performance of the signature derived from a cohort was different when applied to other cohorts, suggesting heterogeneity in gene expression across different populations [24,42]. Thus, these performances need to be validated by testing the generalized population with variable genetic backgrounds, diverse strains of MTB, and different environmental exposures [18,42]. Furthermore, transcriptional signatures can also be affected by individual characteristics such as age, immunosuppressive condition, and other comorbidities. Therefore, further assessment of these potential confounding factors is required for identifying a universal signature [25,26].
All studies showed that the predictive performance declined with increasing time intervals prior to disease development. Thus, transcriptomic biomarkers reflect short-term risk of TB [25,42]. These limitations may lead to consideration of an optimal testing strategy during the potential risk period, such as the current follow-up strategy for lung nodules. In the context of existing evidence, serial testing among selected high-risk groups may be necessary [25].
To facilitate the implementation of novel RNA signatures as point-of-care tests, many steps are required. These barriers include a small number of target transcriptional genes, technical issues involved in RNA extraction, RT-PCR, platform development of selected signature gene transcripts, and low cost [24,42].
Finally, gene signature-guided TB preventive therapy resulted in an insufficient reduction in the development of incident TB [27], although the weekly 3HP regimen adopted in that study was an effective one endorsed by the WHO. If a gene expression signature predicts incipient TB, individuals with such gene expression may have a greater mycobacterial burden or have different metabolic states compared to those with general LTBI detected by IGRA. Thus, existing preventive regimens may not be effective under these altered circumstances. Further research is required to evaluate whether the current TB preventive therapy is appropriate for the management of individuals targeted by predictive blood RNA signatures.
Conclusion
We have briefly summarized the recent progress in the blood transcriptomic approach in terms of risk prediction for future progression to TB. The performance of novel RNA signatures for the prediction of incident TB within 2 years was more modest than expected. However, some signatures showed convincing accuracy in predicting short-term risk for 3 to 6 months. If an easy-to-use platform to detect these RNA signatures is developed, its periodic testing every 3 to 6 months can be adopted during the period over which a significant risk of progression to TB exists. Further studies are required to evaluate whether currently available TB preventive therapy regimens are effective in reducing TB incidence in individuals based on gene signatures or whether relevant RNA expression returns to normal levels after completion of TB preventive therapy. Recent advances have been made in TB detection technology using non-sputum samples, such as the Xpert MTB Host Response prototype. Now, we are looking forward to developing a novel host blood gene-based predictive test that can change LTBI management strategies in the near future.
Notes
Authors’ Contributions
Conceptualization: Kim CH, Lee J. Methodology: Kim CH, Choi G, Lee J. Investigation: Kim CH, Lee J. Writing-original draft preparation: Kim CH, Choi G. Writing-review and editing: Lee J. Approval of final manuscript: all authors.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Funding
No funding to declare.