3. Alberti C, Bouakline A, Ribaud P, Lacroix C, Rousselot P, Leblanc T, et al. Relationship between environmental fungal contamination and the incidence of invasive aspergillosis in haematology patients. J Hosp Infect 2001;48:198-206.


4. Oren I, Haddad N, Finkelstein R, Rowe JM. Invasive pulmonary aspergillosis in neutropenic patients during hospital construction: before and after chemoprophylaxis and institution of HEPA filters. Am J Hematol 2001;66:257-62.


5. Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest 2002;121:1988-99.


6. Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax 2015;70:270-7.


7. Fernandez-Ruiz M, Silva JT, San-Juan R, de Dios B, GarciaLujan R, Lopez-Medrano F, et al.
Aspergillus tracheobronchitis: report of 8 cases and review of the literature. Medicine (Baltimore) 2012;91:261-73.

8. Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van Wijngaerden E. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med 2004;170:621-5.


9. Guinea J, Torres-Narbona M, Gijon P, Munoz P, Pozo F, Pelaez T, et al. Pulmonary aspergillosis in patients with chronic obstructive pulmonary disease: incidence, risk factors, and outcome. Clin Microbiol Infect 2010;16:870-7.


10. Cho BH, Oh Y, Kang ES, Hong YJ, Jeong HW, Lee OJ, et al.
Aspergillus tracheobronchitis in a mild immunocompromised host. Tuberc Respir Dis 2014;77:223-6.

11. Youssif SF, Hassan EA, Moharram AM, Farhan MA, Badary DM, Hasan AAA. Is bronchoscopic view a reliable method in diagnosis of tracheobronchial aspergillosis in critically ill non-neutropenic patients? Clin Respir J 2020;14:956-64.


12. Nyga R, Maizel J, Nseir S, Chouaki T, Milic I, Roger PA, et al. Invasive tracheobronchial aspergillosis in critically ill patients with severe influenza: a clinical trial. Am J Respir Crit Care Med 2020;202:708-16.


13. Wu N, Huang Y, Li Q, Bai C, Huang HD, Yao XP. Isolated invasive
Aspergillus tracheobronchitis: a clinical study of 19 cases. Clin Microbiol Infect 2010;16:689-95.


14. Husain S, Kwak EJ, Obman A, Wagener MM, Kusne S, Stout JE, et al. Prospective assessment of Platelia
Aspergillus galactomannan antigen for the diagnosis of invasive aspergillosis in lung transplant recipients. Am J Transplant 2004;4:796-802.


15. De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 2008;46:1813-21.


16. Singh N, Husain S.
Aspergillus infections after lung transplantation: clinical differences in type of transplant and implications for management. J Heart Lung Transplant 2003;22:258-66.


17. Cha SI, Shin KM, Yoo SS, Jeong JY, Yoon GS, Lee SY, et al. Pseudomembranous
Aspergillus tracheobronchitis in an immunocompetent patient. Tuberc Respir Dis 2008;65:400-4.

18. Park BJ, Kim YK, Kim H, Kim Y, Lee HI, Kang HM, et al. A case of endobronchial aspergillosis completely obstructing lobar bronchus. Tuberc Respir Dis 2005;59:311-4.

20. Kramer MR, Denning DW, Marshall SE, Ross DJ, Berry G, Lewiston NJ, et al. Ulcerative tracheobronchitis after lung transplantation: a new form of invasive aspergillosis. Am Rev Respir Dis 1991;144:552-6.


21. Sakaguchi K, Koga Y, Yagi T, Nakahara T, Todani M, Fujita M, et al. Severe fever with thrombocytopenia syndrome complicated with pseudomembranous
Aspergillus tracheobronchitis in a patient without apparent risk factors for invasive aspergillosis. Intern Med 2019;58:3589-92.



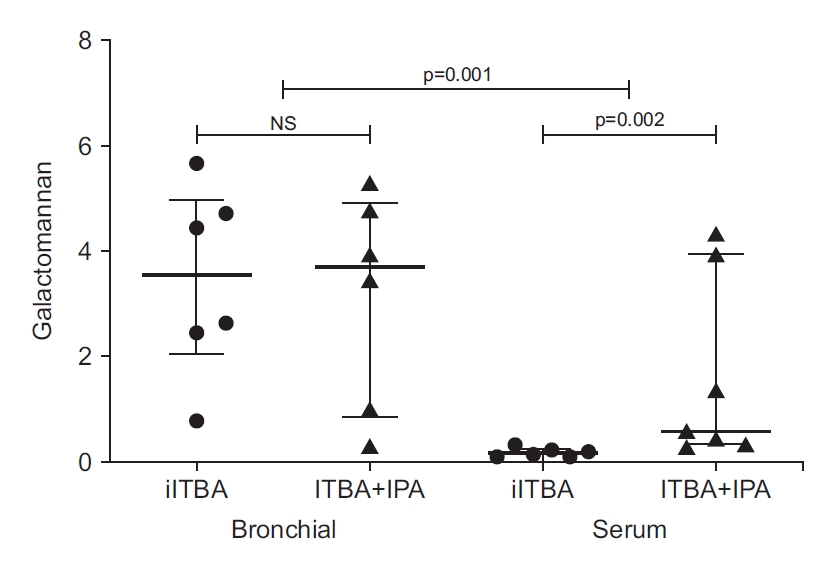
22. Heng SC, Chen SC, Morrissey CO, Thursky K, Manser RL, De Silva HD, et al. Clinical utility of
Aspergillus galactomannan and PCR in bronchoalveolar lavage fluid for the diagnosis of invasive pulmonary aspergillosis in patients with haematological malignancies. Diagn Microbiol Infect Dis 2014;79:322-7.


23. Husain S, Paterson DL, Studer SM, Crespo M, Pilewski J, Durkin M, et al.
Aspergillus galactomannan antigen in the bronchoalveolar lavage fluid for the diagnosis of invasive aspergillosis in lung transplant recipients. Transplantation 2007;83:1330-6.


24. van Assen S, Bootsma GP, Verweij PE, Donnelly JP, Raemakers JM.
Aspergillus tracheobronchitis after allogeneic bone marrow transplantation. Bone Marrow Transplant 2000;26:1131-2.


25. Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis 2006;42:1417-27.


26. van de Groep K, Verboom DM, van de Veerdonk FL, Haas PA, van der Poll T, Schultz MJ, et al. Detection of invasive aspergillosis in critically ill patients with influenza: the role of plasma galactomannan. Am J Respir Crit Care Med 2019;200:636-8.


29. Chang CC, Athan E, Morrissey CO, Slavin MA. Preventing invasive fungal infection during hospital building works. Intern Med J 2008;38:538-41.


30. Talento AF, Fitzgerald M, Redington B, OŌĆÖSullivan N, Fenelon L, Rogers TR. Prevention of healthcare-associated invasive aspergillosis during hospital construction/renovation works. J Hosp Infect 2019;103:1-12.









 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



