 |
 |
| Tuberc Respir Dis > Volume 82(3); 2019 > Article |
|
Abstract
Background
Methods
Results
Notes
Authors' Contributions:
Conceptualization: Choi H, Kim HJ.
Methodology: Choi H.
Software: Oh KH.
Validation: Kim HJ.
Formal analysis: Choi H, Kim H, Oh KH.
Investigation: Oh HW.
Data curation: Kim H.
Writing - original draft preparation: Kim H.
Writing - review and editing: Choi H, Kim HJ, Oh KH, Oh HW.
Approval of final manuscript: all authors.
References
Figure 1
Cascade analysis of tuberculosis (TB) screening project involving the elderly who live in the Jeollanam-do region. PCR: polymerase chain reaction.
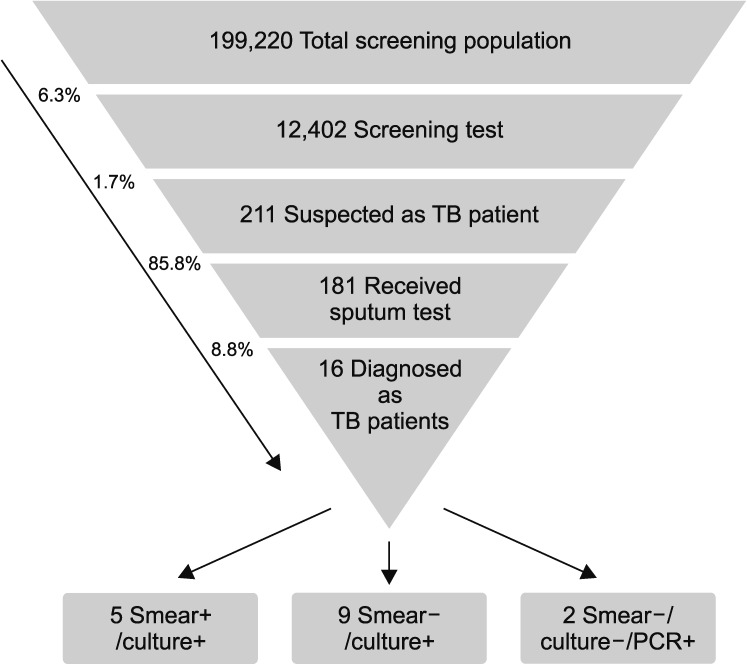
Table 1
Differences in the prevalence rates for cases suspected of TB and those diagnosed with TB depending on various demographic and clinical characteristics
Table 2
Comparison of the TB notification rate between the “2009 and 2014 cohort of newly notified TB cases” and the “2017 TB screening for the elderly people living in the JN region”
*Choi HJ (2017). Development of a pilot model for TB management and care for socioeconomically vulnerable regions and groups. Cheongju: Korea Centers for Disease Control and Prevention14. †Odds ratios were calculated using chi-square tests.
TB: tuberculosis; JN: Jeollanam-do.
Table 3
Comparison of the results of the TB screening project conducted in the Jeollanam-do region: “annual TB screening program for vulnerable populations” and “2017 TB screening for the elderly”
*Korean National Tuberculosis Association (2017). Korean National Tuberculosis Association annual report 2016. Seoul: Korean National Tuberculosis Association15, with permission of Korean National Tuberculosis Association.
TB: tuberculosis.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




