 |
 |
| Tuberc Respir Dis > Volume 76(6); 2014 > Article |
|
Abstract
Primary tracheal amyloidosis (PTA) can lead to airway obstructions, and patients with severe PTA should undergo bronchoscopic interventions in order to maintain airway patency. Focal airway involvements with amyloidosis can only be treated with mechanical dilatation. However, the PTA with diffused airway involvements and concomitant cartilage destructions requires stent placement. Limited information regarding the usefulness of silicone stents in patients with PTA has been released. Therefore, we report a case of diffused PTA with tracheomalacia causing severe cartilage destruction, which is being successfully managed with bronchoscopic interventions and silicone stent placements.
Primary tracheal amyloidosis (PTA) is a very rare form of amyloidosis. The most common presenting symptom is dyspnea caused by deposition of insoluble protein fibrils in the central airway walls1,2. This severe disease can develop respiratory failure requiring aggressive intervention, including intubation and mechanical ventilation, to maintain airway patency.
Bronchoscopic intervention restores airway patency in patients with benign airway obstruction, such as post-intubation and post-tuberculosis stenosis3,4. Several reports have described the outcomes from bronchoscopic intervention in patients with PTA5,6. However, scant information regarding the usefulness of silicone stent placement in patients with PTA is available. Herein, we report a case of diffuse PTA with tracheomalacia causing severe cartilage destruction that was managed successfully by bronchoscopic intervention and the placement of a silicone stent.
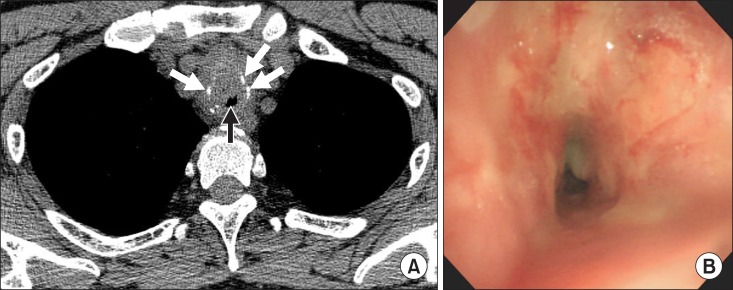
A 48-year-old male presented to the emergency department with respiratory distress. He complained of progressive dyspnea of 2 weeks' duration, and endotracheal intubation was performed due to impending respiratory failure. A chest computed tomography scan revealed luminal narrowing, irregular wall thickening, and severe cartilage destruction in the trachea (Figure 1A).
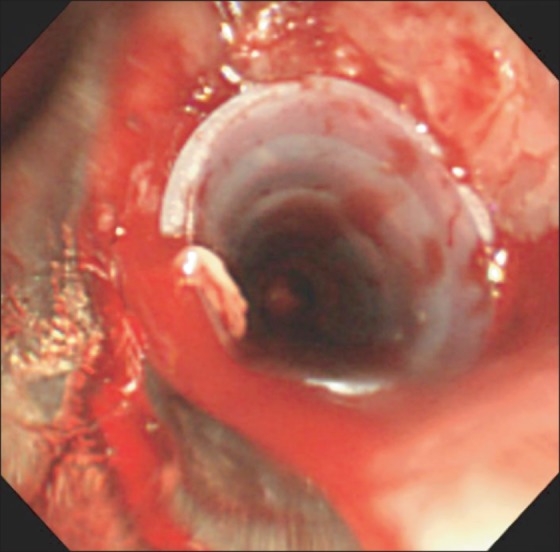
To evaluate the tracheobronchial tree and restore airway patency, rigid bronchoscopy was performed. Initial bronchoscopic findings showed circumferential airway narrowing with exudate (Figure 1B). Ballooning (Boston Scientific, Natick, MA, USA) was performed to mechanically dilate the narrowed airway, and a large amorphous mass was resected by bougienation using the bevel of the rigid bronchoscope (Karl-Storz, Tuttlingen, Germany). After airway dilatation, severe tracheomalacia, causing cartilage destruction and fragmentation, was noted. A silicone airway stent (TNO, Seoul, Korea) was placed to maintain airway patency (Figure 2).
The pathological samples obtained from the tracheal lesions showed fibrosis and amorphous eosinophilic material that selectively stained with Congo Red. Thus, a diagnosis of tracheobronchial amyloidosis was confirmed (Figure 3). The patient experienced symptomatic improvement immediately following rigid bronchoscopy with stenting and was discharged 3 days after the intervention. There were no respiratory symptoms or procedure-related complications during the 6-month follow-up period. A normal pulmonary function test was reported 6 months following bronchoscopic intervention.
Although amyloidosis rarely involves the respiratory tract, life-threatening airway obstruction can develop in patients with severe PTA7. To prevent respiratory arrest and maintain airway patency, bronchoscopic intervention using a rigid bronchoscope is essential. Focal airway involvement can be treated with mechanical dilatation using laser cauterization, ballooning, or bougienage6. However, complex PTA with diffuse airway involvement and concomitant cartilage destruction leads to the loss of airway wall structural integrity. In these cases, airway stent implantation should follow mechanical dilatation.
Recently, a self-expanding metal stent was reported as a possible treatment for severe PTA8. However, metallic stents exert a significant radial force on the tracheal wall and integrate into the airway. This may lead to stent-related complications such as granulation tissue overgrowth, stent fracture, and erosion into the great vessels or the esophagus9,10. The United States Food and Drug Administration has issued a warning for metallic stents in the treatment of benign airway disease due to these complications10. Silicone stents are a reasonable treatment option when an airway stent is indicated for PTA.
The patient had PTA with destruction and fragmentation of the tracheal cartilage. Therefore, mechanical dilatation alone was insufficient to maintain tracheal lumen patency. A silicone stent was placed; this stabilized the patient. Pulmonary function tests remained normal during the 6-month follow-up period. This case demonstrates that silicone airway stenting is a useful and safe therapeutic strategy for patients with severe PTA and intractable airway malacia.
Acknowledgements
We would like to thank Hee Jin Bae (Samsung Medical Center, Seoul, Korea) for editorial assistance.
References
1. Gillmore JD, Hawkins PN. Amyloidosis and the respiratory tract. Thorax 1999;54:444-451. PMID: 10212113.



2. Piazza C, Cavaliere S, Foccoli P, Toninelli C, Bolzoni A, Peretti G. Endoscopic management of laryngo-tracheobronchial amyloidosis: a series of 32 patients. Eur Arch Otorhinolaryngol 2003;260:349-354. PMID: 12937908.



3. Ryu YJ, Kim H, Yu CM, Choi JC, Kwon YS, Kwon OJ. Use of silicone stents for the management of post-tuberculosis tracheobronchial stenosis. Eur Respir J 2006;28:1029-1035. PMID: 16971412.


4. Park HY, Kim H, Koh WJ, Suh GY, Chung MP, Kwon OJ. Natural stent in the management of post-intubation tracheal stenosis. Respirology 2009;14:583-588. PMID: 19383113.


5. Berraondo J, Novella L, Sanz F, Lluch R, de Casimiro E, Lloret T. Management of tracheobronchial amyloidosis with therapeutic bronchoscopic techniques. Arch Bronconeumol 2013;49:207-209. PMID: 23347550.


6. Alloubi I, Thumerel M, Begueret H, Baste JM, Velly JF, Jougon J. Outcomes after bronchoscopic procedures for primary tracheobronchial amyloidosis: retrospective study of 6 cases. Pulm Med 2012;2012:352719PMID: 23326661.




7. Howard ME, Ireton J, Daniels F, Langton D, Manolitsas ND, Fogarty P, et al. Pulmonary presentations of amyloidosis. Respirology 2001;6:61-64. PMID: 11264765.


8. Fiorelli A, Accardo M, Galluccio G, Santini M. Tracheobronchial amyloidosis treated by endobronchial laser resection and self expanding Y stent. Arch Bronconeumol 2013;49:303-305. PMID: 23474207.


9. Stephens KE Jr, Wood DE. Bronchoscopic management of central airway obstruction. J Thorac Cardiovasc Surg 2000;119:289-296. PMID: 10649204.


10. Lund ME, Force S. Airway stenting for patients with benign airway disease and the Food and Drug Administration advisory: a call for restraint. Chest 2007;132:1107-1108. PMID: 17934107.


Figure┬Ā1
Initial computed tomography (CT) and bronchoscopic findings with primary tracheal amyloidosis. (A) On the chest CT scan, the mid-trachea was narrowed to ~3 mm (black arrow) with irregular thickening of the wall and destructions of the tracheal cartilage (white arrows). (B) On bronchoscopy, diffused luminal narrowing secondary to submucosal infiltration was found from the level of thoracic inlet to the lower trachea.
Figure┬Ā2
Silicone stent implantation in a patient with primary tracheal amyloidosis. A silicone airway stent (outer diameter 12 mm, inner diameter 10 mm, length 50 mm) was inserted into the trachea to maintain airway patency.
Figure┬Ā3
Histological examinations of the bronchoscopic biopsy. (A) There is a homogenous pink amorphous material in the subepithelial region (H&E stain, ├Ś100). (B) The subepithelial amorphous material shows reactivities with the amyloid P stain (amyloid P stain, ├Ś100). (C) Congo Red staining reveals apple-green birefringence under the polarized light (Congo Red, ├Ś200).

- TOOLS


 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation




