Introduction
Weaning failure is associated with prolonged mechanical ventilation and intensive care unit (ICU) stay as well as increased hospital mortality ranging between 40% and 50% [
1,
2]. Delay in weaning from ventilator increases the inherent risks of mechanical ventilation, such as barotrauma, ventilatorassociated pneumonia, and ventilator-induced diaphragmatic atrophy. On the other hand, premature discontinuation of mechanical ventilation is equally as harmful and associated with mortality rates of about 42% [
3]. Therefore, discontinuing mechanical ventilation in a timely and safe manner is of major importance, and strategies that assist in discontinuation should be thoroughly evaluated [
4].
Many weaning parameters have been used to predict weaning failure, including rapid shallow breathing index (RSBI) which is the ratio of respiratory frequency to tidal volume, minute ventilation, maximum inspiratory pressure, tracheal airway occlusion pressure of 0.1 second (P 0.1), dynamic compliance (Cdyn), respiratory rate (RR), oxygenation, maximum inspiratory pressure, and dynamic compliance, respiratory rate, oxygenation, maximum inspiratory pressure (CROP) index, but none has shown great prognostic accuracy [
5]. Moreover, these parameters do not directly reflect diaphragmatic function, which is measured by diaphragmatic thickness fraction (DTF) and diaphragmatic excursion (DE) [
6].
The diaphragm is the principal respiratory muscle in humans and is subjected to various adverse factors in critical patients, such as hypoxia, sepsis, electrolyte imbalance, and neuromuscular blocking agents in addition to mechanical ventilation, which causes ventilator-induced diaphragmatic dysfunction by decreasing the force-generating capacity of the diaphragm [
7]. Several diaphragm function evaluation techniques have been previously investigated, such as fluoroscopy [
8], phrenic nerve stimulation [
9], dynamic magnetic resonance imaging [
10], and trans-diaphragmatic pressure measurement [
11]. However, the cumbersome nature of these techniques, ionizing radiation exposure, invasiveness, and need for patient transportation has limited their widespread use [
12]. In contrast to those methods, ultrasound is ionizing radiation-free, noninvasive, inexpensive, and available at bedside, so it is a useful technique for assessment of the dynamic and structural function of the diaphragm. Several ultrasound techniques, such as B-mode and M-mode, have been used to assess diaphragm sonographic predictors: DE, which measures the distance that the diaphragm is able to move during the respiratory cycle, and DTF, which is the ratio between the difference in thickness from inspiration and expiration divided by the thickness on expiration [
13]. DTF and DE during respiration reflect diaphragm function. However, the results are controversial, and some studies have reported that DE and DTF had high sensitivity and specificity in predicting weaning outcome [
14].
The aim of the study was to determine if measurement of diaphragmatic function by ultrasound may be used to predict successful extubation and to determine cut-off values for predicting success or failure of extubation. We also evaluated the performance of these ultrasound parameters in comparison with conventional parameters routinely used to predict successful weaning from mechanical ventilation.
Materials and Methods
This study was conducted in 62 patients who were mechanically ventilated in the respiratory ICU, Department of Chest Medicine, Kasr Al-Aini Hospital, Cairo University between September 2017 and January 2019. The study was approved by the institutional review board at Kasr Al-Aini Hospital, Cairo University (IRB #N-93-2018) and informed consent was obtained from the relatives of all enrolled patients. Patients who were mechanically ventilated invasively for more than 48 hours and fulfilled the criteria of weaning (hemodynamic stability, RR <35 breaths per minute, and hemoglobin level >7 g/dL) [
5] and succeeded the spontaneous breathing trial (SBT) were included in the study. Patients with diaphragmatic paralysis proved by transthoracic ultrasound and patients with neuromuscular diseases, such as muscular dystrophy, poliomyelitis, and myasthenia gravis, were excluded from the study.
Demographics, clinical information, and Acute Physiology and Chronic Health Evaluation II (APACHE II) score were recorded on admission.
The patients were ventilated using volume-controlled ventilation (tidal volume [TV]=6 mL/kg). Assessment of lung mechanics while the patients were on mechanical ventilation was performed by recording the tidal volume, RR, RSBI calculated by dividing the RR on tidal volume, static compliance (Cstat) calculated by dividing the TV on plateau pressure minus positive end expiratory pressure, and Cdyn calculated by dividing the TV on peak pressure minus positive end expiratory pressure.
Diaphragms were visualized by ultrasound during an SBT.
All transthoracic ultrasound (Logiq P3, GE Healthcare, Chicago, IL, USA) evaluations were performed with the patients in a semi-sitting position exposing the chest and abdomen to look for the following:
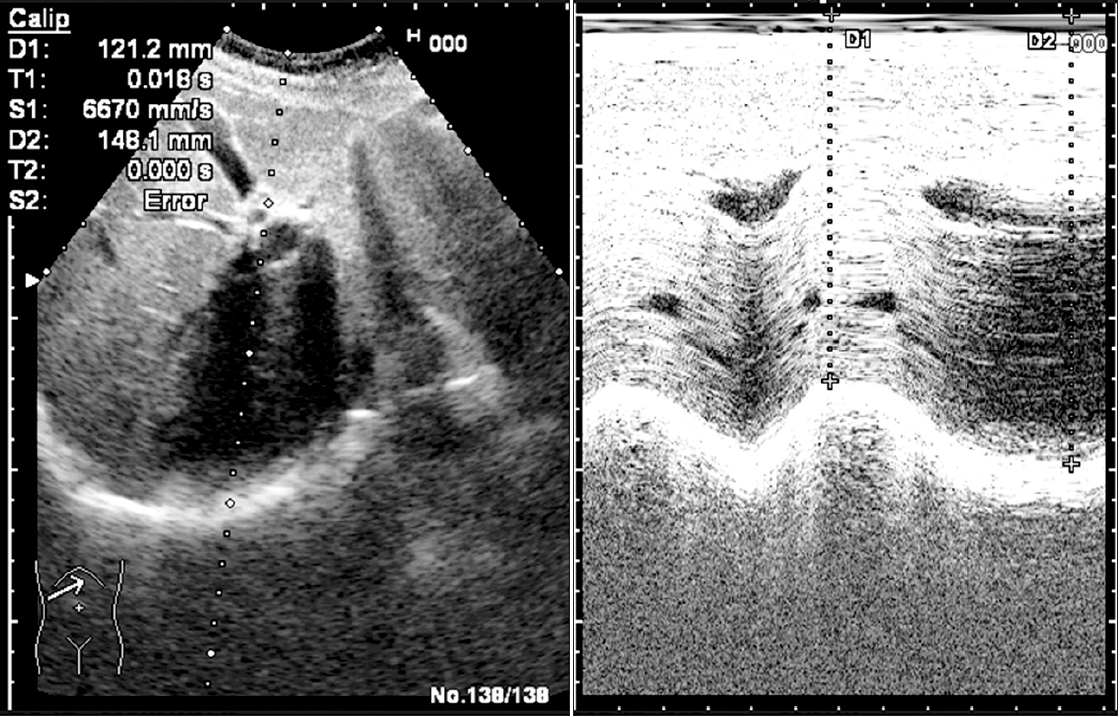
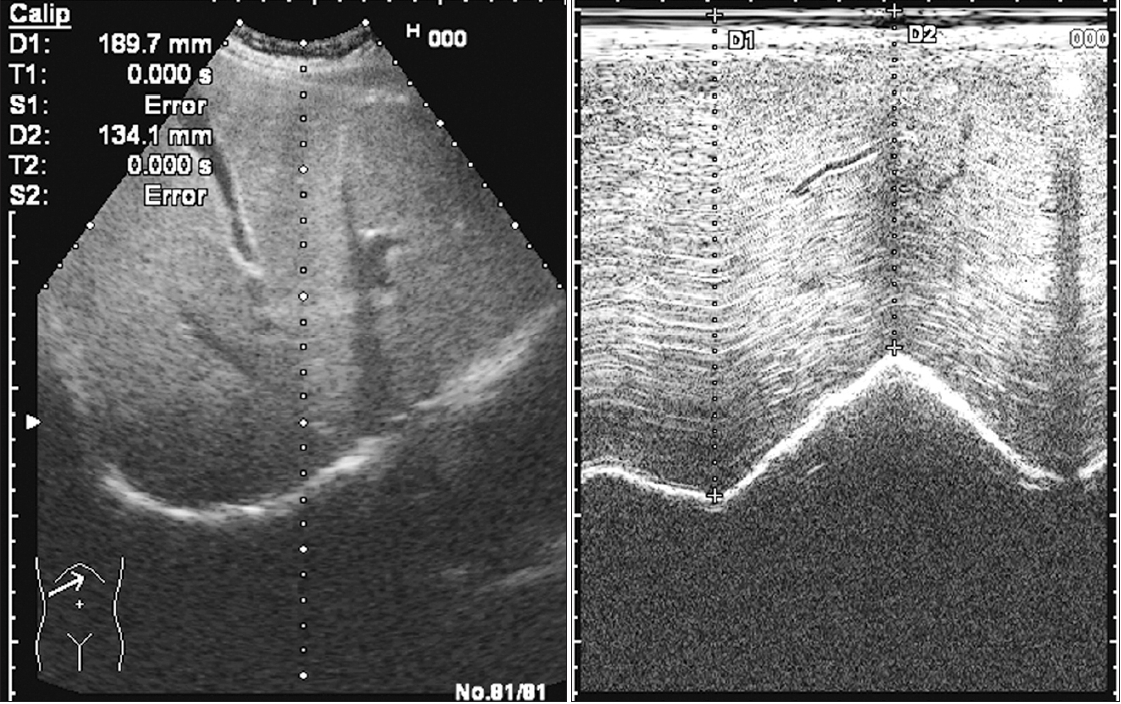
1. Diaphragmatic excursion
A curvilinear transducer using the low-frequency of 3.5 MHz was placed on the right sub-costal angle between the midclavicular line and anterior axillary line during quiet breathing and directed medially, cranially, and dorsally to achieve the best view of the right hemidiaphragm by using the liver as a window. The movements of the right hemidiaphragms were recorded by M-mode sonography in real time. After ensuring quiet regular breathing by the patient, we froze the sonogram. During M-mode imaging, the normally functioning diaphragm is represented as an echogenic line that moves freely during inspiration and expiration. Inspiration is identified on the sonographic tracing as upward flexion (during inspiration, there is downward movement of the diaphragm: i.e., toward the probe, leading to upward flexion of the tracing) (
Figures 1,
2). Expiration is identified as downward flexion (during expiration, there is upward movement of the diaphragm: i.e., away from the probe, leading to downward flexion of the tracing toward the baseline; the baseline represents the expiratory pause that follows expiration).
On the M-mode images, the distances between the probe and copula during inspiration and resting expiration were measured, and the difference between the two distances equaled the DE range (
Figures 1,
2).
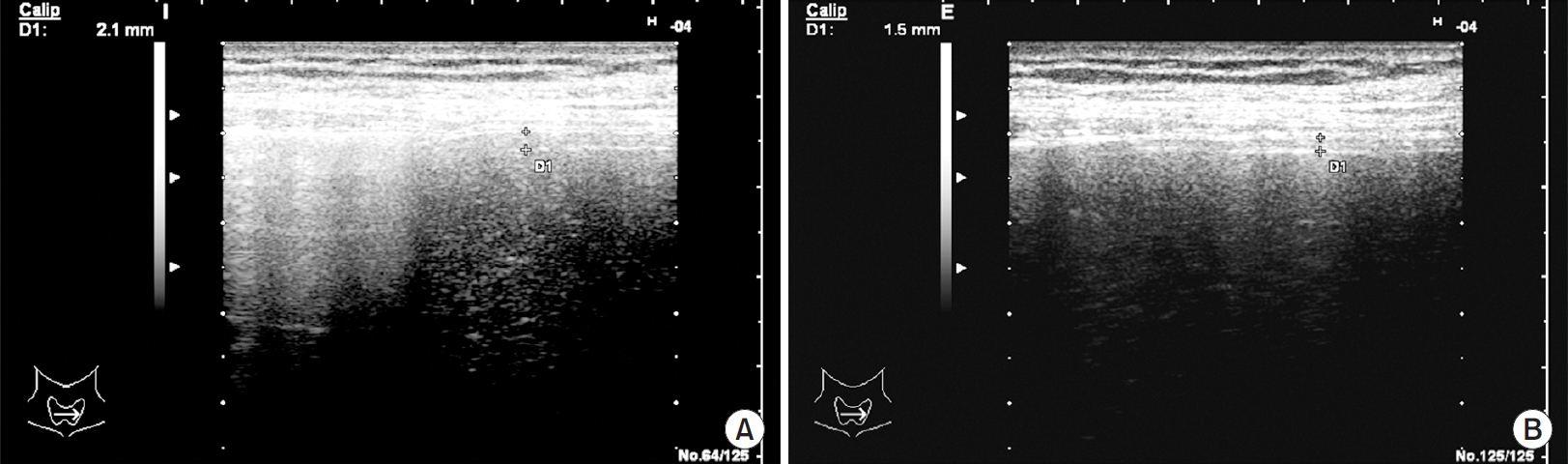
2. Diaphragmatic thickness
High-frequency linear probe with a frequency of 7-12 MHz was used to measure the diaphragm thickness (DT) at the zone of apposition. The patient was placed in a semisitting position. The probe was placed at the anterior axillary line in the longitudinal plane between the seventh and ninth intercostal spaces to measure the DT. The liver window was used to visualize the diaphragm. The right DT was measured as there was no significant difference in thickness between the right and left sides. On B-mode imaging, the diaphragm appears as a thick echogenic linear structure between highly reflective pleural and peritoneal membranes. Thickness was measured by placing calipers on reflective lines at the end of inspiration and expiration (
Figure 3). Thickness at end inspiration (Insp DT) as well as thickness at end expiration (Exp DT) were measured. The DTF was calculated according to the following formula:
DTF=[(Insp DTŌłÆExp DT)/Exp DT]├Ś100
Patients were extubated when able to tolerate the SBT for 2 hours without exhibiting clinical signs of respiratory fatigue (increase in RR >30 breaths per minute, heart rate >120 beats per minute, systolic blood pressure <90 mm Hg or >180 mm Hg, presence of confusion, agitation, diaphoresis, cyanosis, or evidence of increasing respiratory effort). The patients were followed until discharge or death.
A successful extubation was defined as spontaneous breathing for >48 hours following extubation. A failed extubation was defined as someone who was reintubated within 48 hours.
The patients were divided into two groups according to their extubation outcome: successfully extubated group and failed extubation group. The two groups were compared according to their age, laboratory results, lung mechanics, duration of mechanical ventilation, APACHE II score, and diaphragmatic function parameters.
3. Statistical analysis
Data was coded and entered by using the statistical package SPSS version 21 (IBM Corp., Armonk, NY, USA). The data were summarized by using number and percentage for qualitative variables. The quantitative data that were normally distributed were TV, Insp DT, and Exp DT. These data were presented by mean and standard deviation. Comparisons between the successful extubation and failed extubation groups regarding these normally distributed data were performed by using the independent sample t test.
The quantitative data that were not normally distributed were age, APACHE score, duration of mechanical ventilation, RR, RSBI, P/F ratio (arterial pressure of oxygen divided by the fraction of inspired oxygen expressed as a decimal), Cdyn, Cstat, DE, and DTF%. These data were presented by median and interquartile range. Comparisons between the successful extubation and failed extubation groups regarding these data that were not normally distributed were performed by using the non-parametrical Mann-Whitney test.
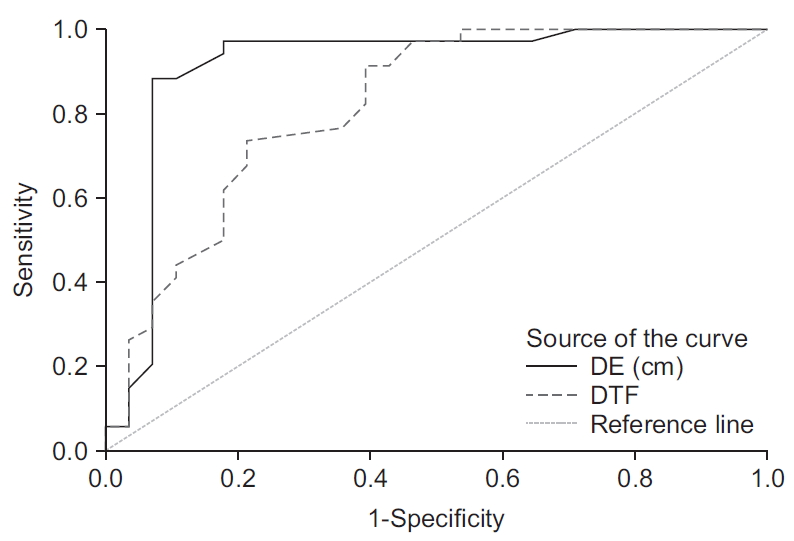
To determine the best cut-off for DE and DTF parameters to predict successful extubation, we calculated area under the receiving operating characteristic curve (ROC).
Correlation analysis was performed to test for linear relationships between variables. We accepted p-values <0.05 as indicative of statistical significance.
Results
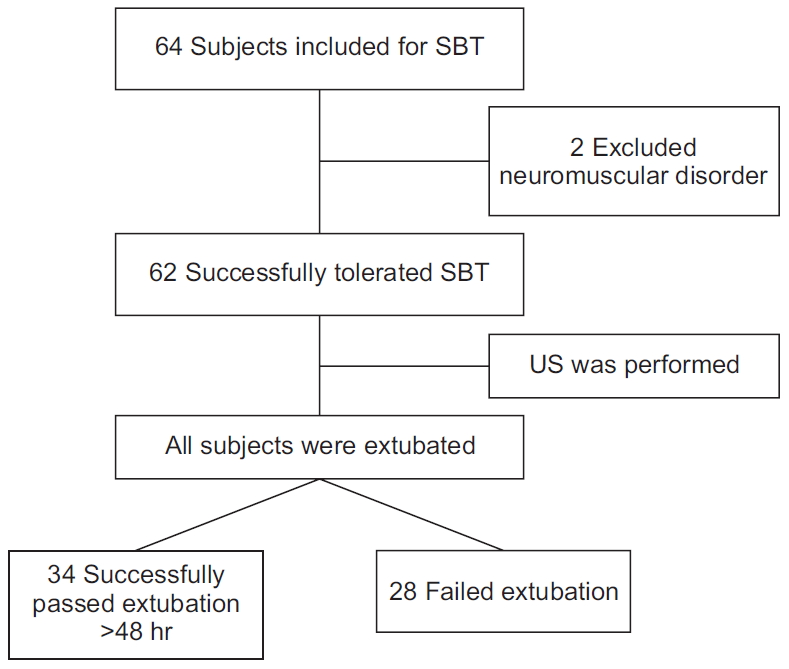
The study included 64 patients who were ready for weaning; two patients showed signs of neuromuscular disorders and were excluded from the study. The remaining 62 patients were subjected to SBT and followed up for 48 hours to record extubation outcome (
Figure 4). There were 26 (41.9%) females and 36 (58.1%) males. The included patients were diagnosed as follows: 15 (24.1%) had chronic obstructive pulmonary disease, 14 (22.5%) had overlap syndrome, 13 (20.9%) had extensive pneumonia, six (9.6%) had interstitial lung disease, four (6.4%) had bronchiectasis, four (6.4%) had sepsis, two (3.2%) had lymphoma, two (3.2%) had mediastinal mass, and two (3.2%) were trauma patients.
As a cause of respiratory failure, 14 patients (22.6%) presented with type 1 respiratory failure, and 48 (77.4%) presented with type 2 respiratory failure.
History of ischemic heart diseases and cardiac problems were encountered in 16 patients (25.8%), and a history of diabetes and metabolic syndrome was found in 15 patients (24.2%).
Out of all patients, 28 (45%) failed extubation and required reintubation and 34 (55%) were successfully extubated and weaned.
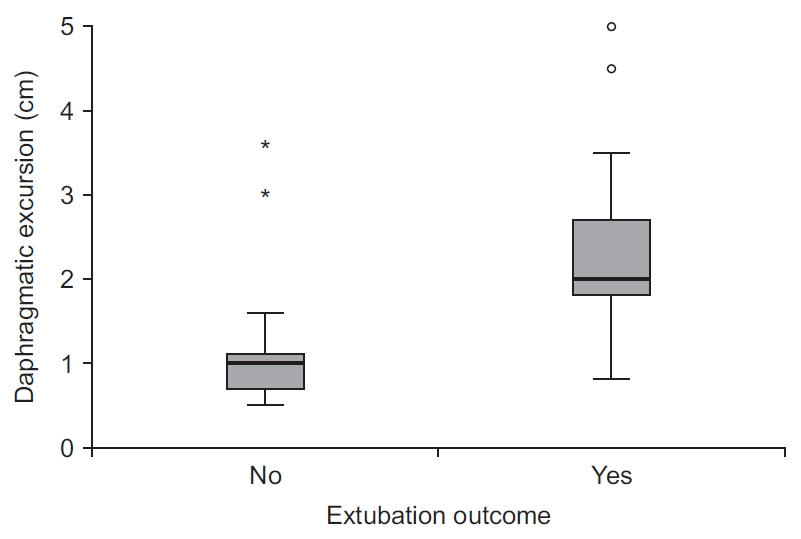
The two groups did not significantly differ in age but differed in APACHE II score, which was significantly lower in the successful extubation group. As expected, the duration of mechanical ventilation was significantly higher in the failed extubation group versus the successful extubation group. As presented in
Table 1, the parameters of lung mechanics represented by Cstat and Cdyn and the diaphragmatic function indices represented by Insp DT and Exp DT, DE, and DTF were significantly higher in the patients who succeeded in the trial of extubation (
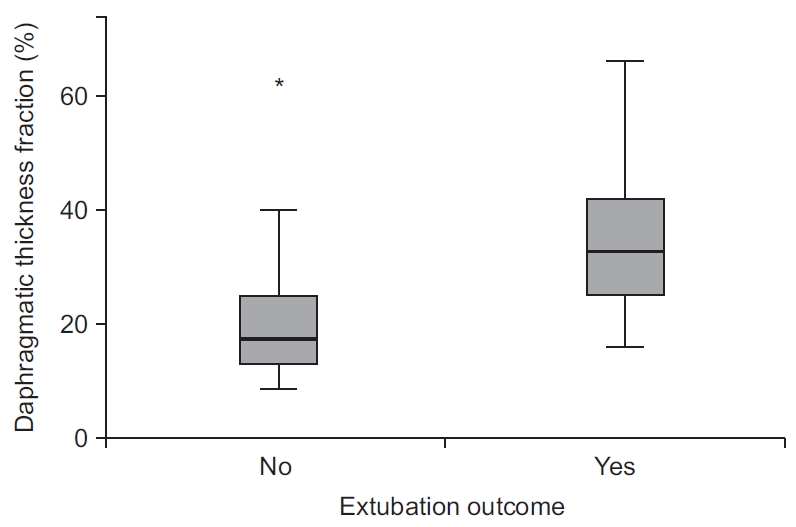
Figures 5,
6).
DE negatively correlated with the APACHE II score (r= ŌłÆ0.384, p=0.002) as well as with the duration of mechanical ventilation (r=ŌłÆ0.494, p<0.001) and positively correlated with dynamic compliance (r=0.267, p=0.036).
DTF negatively correlated with duration of mechanical ventilation (r=ŌłÆ0.373, p=0.003) and positively correlated with dynamic compliance (r=0.266, p=0.037).
A ROC curve was used to assess the accuracy of DE and DTF in predicting weaning outcome. A cut-off value of DE of >1.25 cm was associated with successful extubation, with a sensitivity of 97% and a specificity of 82%. A DTF of >21.5% predicts successful extubation with a sensitivity of 91.2% and a specificity of 60.7% (
Figure 7).
Discussion
The process of weaning from mechanical ventilation is complex, with an estimated failure rate of 20% [
14].
The diaphragm is considered to be the main muscle of respiration because it contributes approximately to 70% of the TV during inspiration in normal people [
15]. Therefore, diaphragmatic dysfunction is one of the most important factors accounting for difficult weaning [
16]. Ultrasound is a readily available, easy to use, and noninvasive imaging modality that is commonly used for procedures and clinical evaluation in the modern ICU [
17]. Recently, ultrasound measurements have been used for evaluation of diaphragmatic contractility either by assessment of DE or DT [
17]. In the current study, we showed that measurements of DE and DTF by ultrasound could be used to predict successful weaning.
The patients were classified into successful extubation group and failed extubation group. There was no statistically significant difference in age between the groups, which meant that age was not a confounding factor that affected the extubation outcome, as would be expected, for example, in sarcopenia, which is age-related muscular loss.
Regarding the APACHE II score, there was a highly significant increase in the failed extubation group (p<0.001) (
Table 1) and a significant negative correlation between the APACHE II score and DE (p=0.002) but not between the APACHE II score and DTF (p=0.053). The APACHE II score contains some parameters that might affect the diaphragmatic function, such as serum potassium, albumin, and hemoglobin levels. These results supported the conclusion that extubation failure was related to causes other than diaphragmatic factors. Additionally, the low significant negative correlation between the APACHE II score and DE and non-significant correlation between the APACHE II score and DTF parameters supported the conclusion that there were no large differences in the parameters affecting the diaphragm level between the two groups [
18]. This finding could also be explained by the idea that DTF represents the number of fibers in the diaphragm, whereas DE represents the diaphragm function that can be affected by various measures included in the APACHE II score and explains why the score is correlated with the DE but not with the DTF.
The duration of mechanical ventilation was significantly different between the two groups (
Table 1). Moreover, there were negative correlations between the duration of mechanical ventilation and DE and DTF. Ferrari et al. [
13] showed a statistically significant decrease in the duration of mechanical ventilation in the weaned group relative to that in the non-weaned group. Goligher et al. [
19] also discussed the same issue and concluded that changes in DT are common during mechanical ventilation and may be associated with diaphragmatic weakness. These results were in accordance with Grosu et al. [
20] where their study revealed that the duration of mechanical ventilation significantly predicted decreases in DT and strength. This finding can be explained by a previous findings that prolonged controlled mechanical ventilation in patients triggered significant reductions in the generation of both active and passive diaphragm myofibrillar force by reducing myofibrillar protein levels [
21] and that the duration of mechanical ventilation was correlated with DT, which also explained our finding above because a significant decrease in inspiratory DT at end inspiration by approximately 17% was observed on the third day of mechanical ventilation. This decrease continued progressively through the course of mechanical ventilation.
Regarding RSBI, there was no statistically significant difference between the two groups (
Table 1) or when correlating RSBI with the DE and DTF. The RSBI is an integrative function of respiratory load and inspiratory muscle capacity that reflects the function of all inspiratory muscles, including the diaphragm, scalenes, para-sterna intercostals, and accessory inspiratory muscles (sternomastoids and external intercostals). If the diaphragm is failing (in a T-piece trial), the nondiaphragm inspiratory muscles will compensate to preserve TV, and the presence of diaphragm weakness may be ŌĆśmaskedŌĆÖ by the increased contribution of the non-diaphragm inspiratory muscles (ŌĆśrib cageŌĆÖ muscles) to TV. However, the rib cage muscles are more fatigable and weaker than the diaphragm and will not be able to sustain adequate ventilation. Accordingly, extubation failure may occur despite an initially acceptable TV and RSBI [
17]. Consequently, RSBI can be considered to be a good parameter to start a weaning trial but not a predictor of weaning success, unlike the diaphragmatic function, which can predict the weaning outcome.
The diaphragm is an active respiratory muscle that contracts during inspiration, and the expiratory phase is passive, so it is main contribution should be at the inspiratory phase. The two groups differed significantly in the end inspiratory thickness of the diaphragm (
Table 1). Comparing our study to that of Ferrari et al. [
13], who examined the DT as a weaning predictor, their study did not find a statistical difference in the DT during total lung capacity or residual volume between the two groups. We measured the DT during quiet breathing unlike in two previous studies [
12,
13], which might explain the different levels of significance, although the numbers did not vary that much.
We found highly significant differences in DE and DTF between the two groups, findings that agree with those of most other recent studies (
Table 1,
Figure 7). Farghaly and Hasan [
16] found that the optimum cut-off of DE that predicted successful weaning was Ōēź10.5 mm, with a sensitivity of 87.5% and a specificity of 71.5%. Kim et al. [
7] determined that a DE <10 mm measured during SBT was associated with weaning failure. Baess et al. [
22] found that a DE >1 cm was a predictor for weaning success. The slight difference in numerical values may be attributed to the different study populations.
DTF was significantly higher in the successful extubation group than in the failed extubation group (
Figure 6). This result is consistent with the studies from Ferrari et al. [
13], DiNino et al. [
17], Dube et al. [
9], and Blumhof et al. [
3], which showed that their DTFs of >36%, >30%, >29%, and >20%, respectively, were consistent with weaning success. These studies also demonstrated the superiority of DTF versus RSBI in predicting weaning outcome, as mentioned above.
In a systematic review [
23] comparing different studies that assessed the contribution of DE and DTF in prediction of weaning outcome and compared the two parameters with each other, DTF was concluded to be superior over DE in prediction of weaning outcome, although in our study we found that DE showed superior sensitivity and specificity to those of DTF. Our finding can be explained by the timing in examining the diaphragm because our study measurements were made during a spontaneous breathing trial without the effect of positive-pressure ventilation. However, in the above-mentioned review, the data were obtained from measurements made during positive-pressure ventilation, which would affect the measured DE that is derived from adding the patientŌĆÖs effort to the pressure generated by the ventilator.
Diaphragmatic ultrasonography was found to be a reliable, noninvasive, and convenient technique for predicting weaning success. Incorporation of DTF and DE in the current weaning protocols will further enhance decision making regarding the optimum time for weaning and should improve weaning outcomes and avoid deleterious effects of prolonged intubations or premature extubations.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



