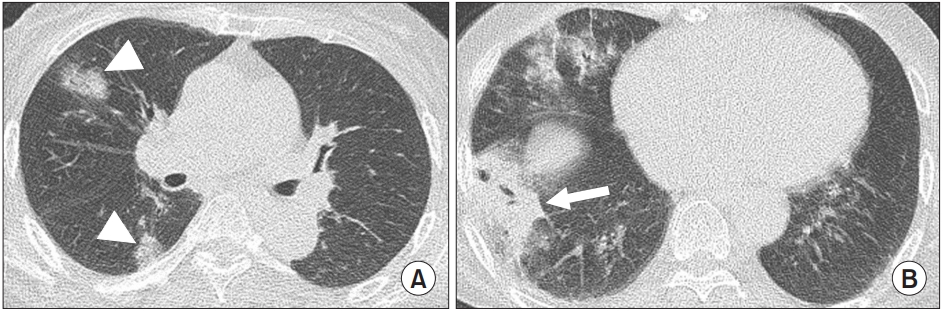
A 72-year-old woman presented to the emergency department of our hospital with altered mental status (10 on the glass coma scale), without a medical history. On her first hospital visit, laboratory tests revealed the following: white blood cell count, 8,300/╬╝L (4,000-10,000); platelet count, 43,000/╬╝L (150,000-450,000); creatinine, 2.0 mg/dL (0.5-0.9); ferritin >1,675.5 ng/mL (4.6-204.0); and C-reactive protein, 12.6 mg/dL (0.0-0.3). The sequential organ failure assessment score was 10 and she was admitted to the intensive care unit. On the second day of admission, severe fever with thrombocytopenia syndrome (SFTS) virus was detected by real-time reverse transcription-polymerase chain reaction. Chest computed tomography (CT) scan, bronchoscopy, and serum aspergillosis antigen test were performed according to our early diagnosis protocol of SFTS-associated pulmonary aspergillosis (SAPA). CT scan images revealed a multifocal consolidative lesion with some cavitation in both lower lungs (
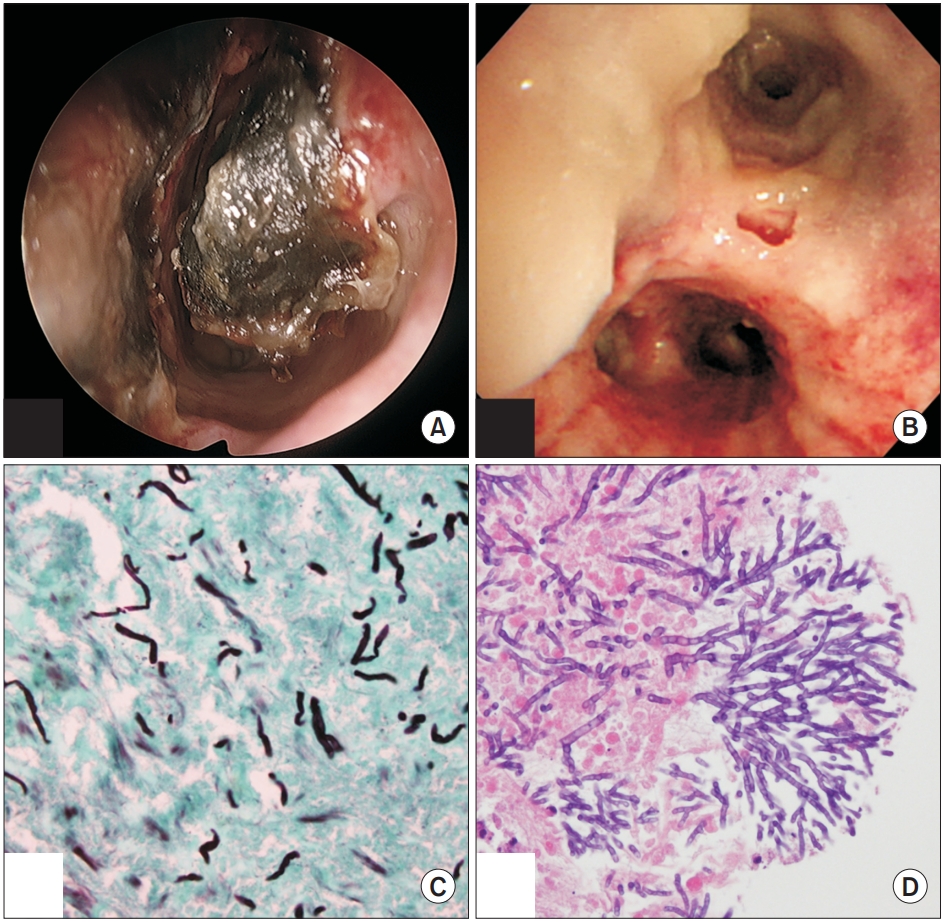
Figure 1). When a bronchoscope was inserted through the left nose, necrotic tissue surrounded by a clot was observed on the nasal septum (
Figure 2A). Bronchoscopy revealed pseudomembranous lesions with some ulceration on the left main and upper lobe bronchus (
Figure 2B). Due to high probability of SAPA, intravenous voriconazole was initiated. In subsequent tests, the serum
Aspergillus antigen level was 4.2 (negative <0.5), and the
Aspergillus species was isolated from bronchoalveolar lavage fluid. On her seventh day in the hospital, tissue specimens from the left nose and the left bronchus confirmed invasive aspergillosis (
Figure 2C,
D). After the treatment with oral voriconazole for 2 months, her clinical course was greatly improved. This study was approved by the Jeju National University Hospital Institutional Review Board (2020-10-00).
The invasive fungal disease may accompany the early clinical course of SFTS [
1,
2], which is associated with poor prognosis [
3,
4]. An invasive nasal and pulmonary aspergillosis was diagnosed in this patient, which had not been reported previously worldwide. For
Aspergillus tracheobronchitis cases without lung lesions [
5], bronchoscopy should be considered. Also, protocolized approach for early diagnosis of SAPA is important.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Print
Print Download Citation
Download Citation



